|
| Topics on Continuous Training |
M. García Lorenzo*, **, S. Melendo Pérez*, P. Soler Palacín*
*Unit of Infectious Pathology and Pediatric Immunodeficiencies. Children’s Hospital, Vall d’Hebron. Barcelona. Spain. **Pediatric Infectious Diseases Unit. Ospedale Luigi Sacco. Milan. Italy
| Abstract
Fever of unknown origin (FUO) in Pediatrics can be defined as an entity in which fever is the main sign, without having reached an etiological diagnosis after more than 7 days, despite the correct performance of the history, physical examination, and first-level complementary tests. |
| Resumen
La fiebre de origen desconocido (FOD) en Pediatría se puede definir como la entidad en que la fiebre es el signo principal, sin haberse alcanzado un diagnóstico etiológico después de más de 7 días, a pesar de la realización correcta de anamnesis, exploración física y pruebas complementarias de primer nivel. |
Key words: Fever of unknown origin; Prolonged fever.
Palabras clave: Fiebre de origen desconocido; Fiebre prolongada.
Pediatr Integral 2023; XXVII (5): 257 – 268
OBJECTIVES
• To distinguish fever of unknown origin from other patterns of prolonged fever.
• To be aware of the most frequent causes of fever of unknown origin in children.
• To carry out a diagnostic approach based on findings in the history and physical examination.
• To recognize differential characteristics of the most common diseases or entities included in the differential diagnosis of fever of unknown origin in Pediatrics.
• To propose a staggered diagnostic algorithm for carrying out complementary tests.
Fever of unknown origin
Introduction
Fever of unknown origin is generally a benign and/or self-limiting entity in children, in which fever is the main sign and in which a diagnosis is not reached after an exhaustive initial evaluation.
Fever of unknown origin (FUO) is a fever of prolonged duration in which the cause cannot be found after at least a week of detailed evaluation. It is a challenging reason for consultation and which, despite being due to a benign and/or self-limiting entity in most cases, can generate great anxiety in the family(1-3).
The differential diagnosis of FUO in Pediatrics includes: infectious diseases, autoimmune or inflammatory diseases, and malignant diseases, among others. In most cases, it is an unusual presentation of a common disease, such as mononucleosis syndromes(4). Other entities, which can cause prolonged fever and that should be considered as the study progresses, may stray from the differential diagnosis included in routine pediatric clinical practice, so it is important to maintain a high index of suspicion and be methodical in the performance of complementary tests(5,6).
The evaluation of FUO requires a detailed history with a thorough review of signs and symptoms to establish its onset and the cardinal features of the disease, as well as a thorough physical examination.
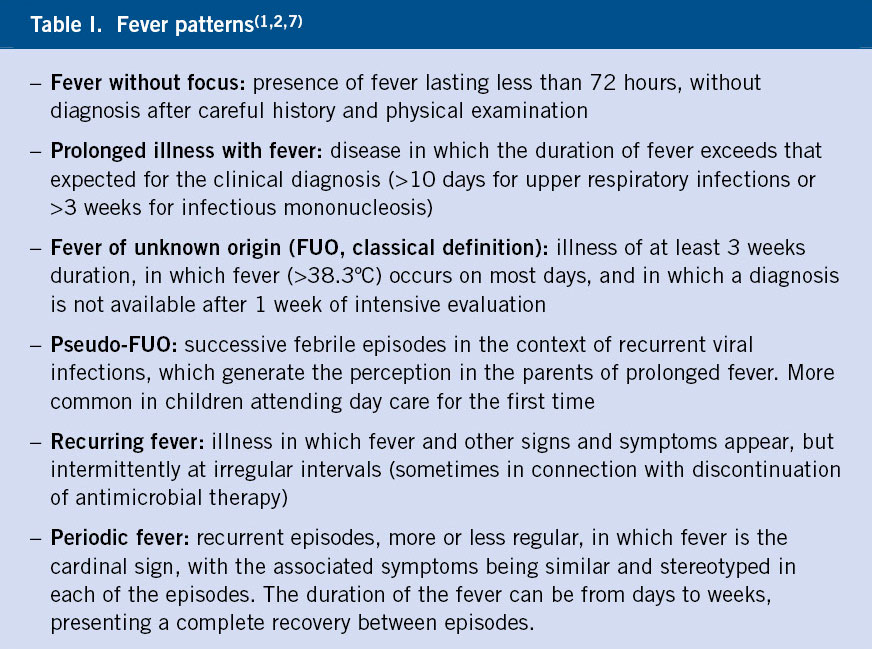
In the history, it is of great importance to confirm the presence of fever, its onset, frequency and pattern, as well as the description of the associated symptoms. The differentiation of the different patterns of fever (Table I) is essential to guide the study within the broad differential diagnosis of prolonged fever, which allows us to reach a diagnosis and finally treat, if necessary, the underlying cause(1).
Physical examination must be complete and systematic, it must include, in addition to the usual examination, the osteoarticular and reticuloendothelial systems (palpation of adenopathies and visceromegaly), as well as a growth assessment(1).
Since many of these cases present with other signs and symptoms, apart from fever, it is advisable to establish a differential diagnosis based on syndromes(5). Complementary tests must be selected in such a way that allow us to confirm or rule out those diseases included in our differential diagnosis. Carrying out a broad study using imaging techniques or serologies of unusual microorganisms, without presenting symptoms or compatible exposure, has low yield(1).
Definition
The classic definition of FUO, which has been used since, especially in the immunocompetent adult population, was published in 1961(8) and defined with 3 criteria: illness lasting >3 weeks of duration, with fever higher than 38.3ºC in several times, and without reaching the diagnosis after 1 week of study in the hospital. This last point was modified years later, accepting 1 week of intensive evaluation without requiring hospitalization in all cases.
In Pediatrics, studies on FUO have used several definitions, varying the degree of temperature to consider fever, its frequency or the total duration necessary, with ranges usually lower than the classic definition: >7 days, between 14 and 21 days or >21 days(9). This makes it difficult to homogenize the studies, observing variations in the frequency of the different etiologies according to the definition used.
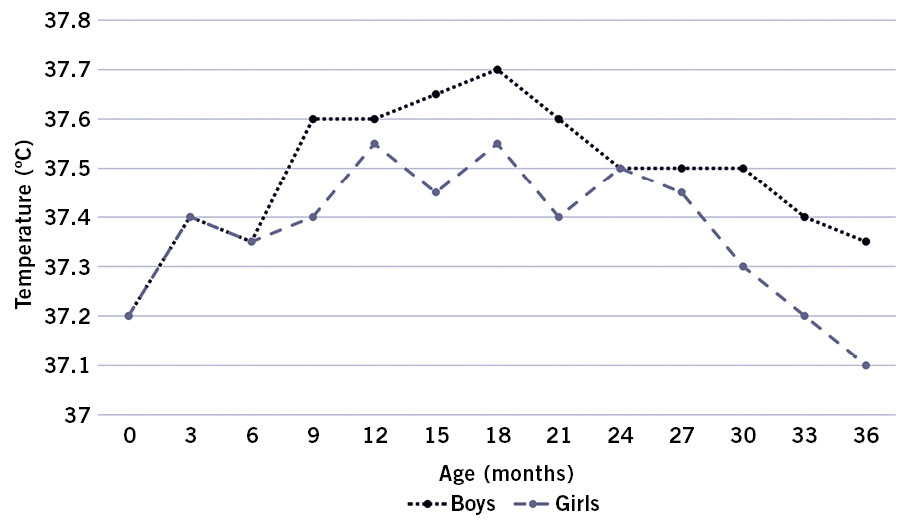
The interpretation of fever should be individualized with nomograms according to the age and sex of the patient (Fig. 1), considering the method used for its measurement. Normal body temperature in children can vary up to 1.5ºC throughout the day, with peak temperatures in the evening hours. This can lead parents to consider as low-grade fever, temperatures that, due to their daily circadian cycle, are within the normal range(1,5).
Figure 1. Normal values of mean rectal temperature for boys and girls up to 36 months. Adapted from: Manthiram K, Edwards KM, Long SS. Prolonged, Recurrent, and Periodic Fever Syndromes. In: Long SS, Prober CG, Fischer M, Kimberlin DW. Principles and Practice of Pediatric Infectious Diseases. 6th ed. Philadelphia: Elsevier; 2023. p. 123-34.
Being consistent with the definition previously used in other publications in our surroundings(3,7,10), we consider fever of unknown origin to be a disease where fever (documented, >38ºC) of more than 7 days duration predominates, with an uncertain diagnosis after an assessment through a detailed medical history, a thorough physical examination, and the performance of first-stage complementary tests.
Etiology
Infections are the most common cause of fever of unknown origin. Not reaching a diagnosis after a correct evaluation is a good predictor of spontaneous resolution.
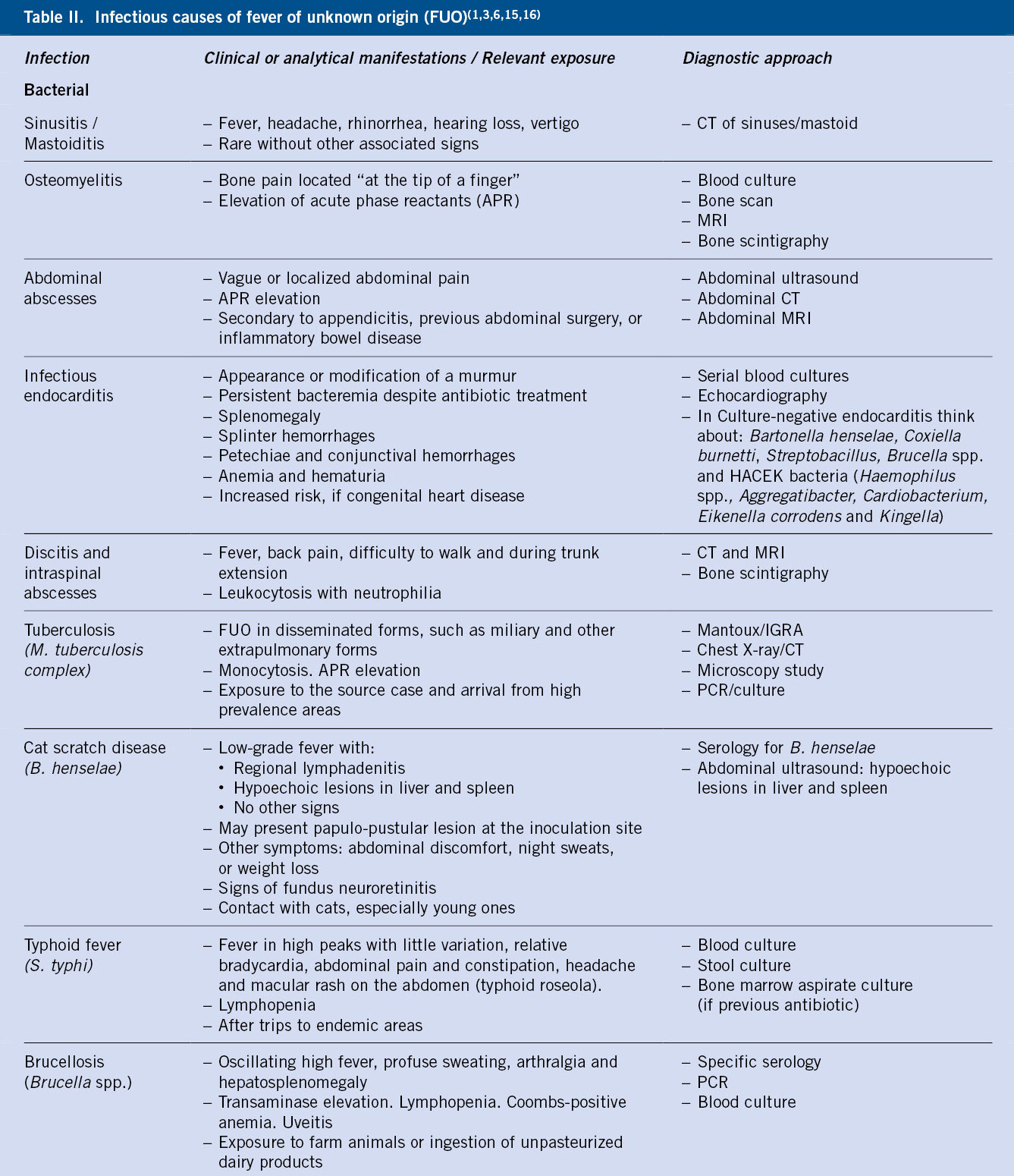
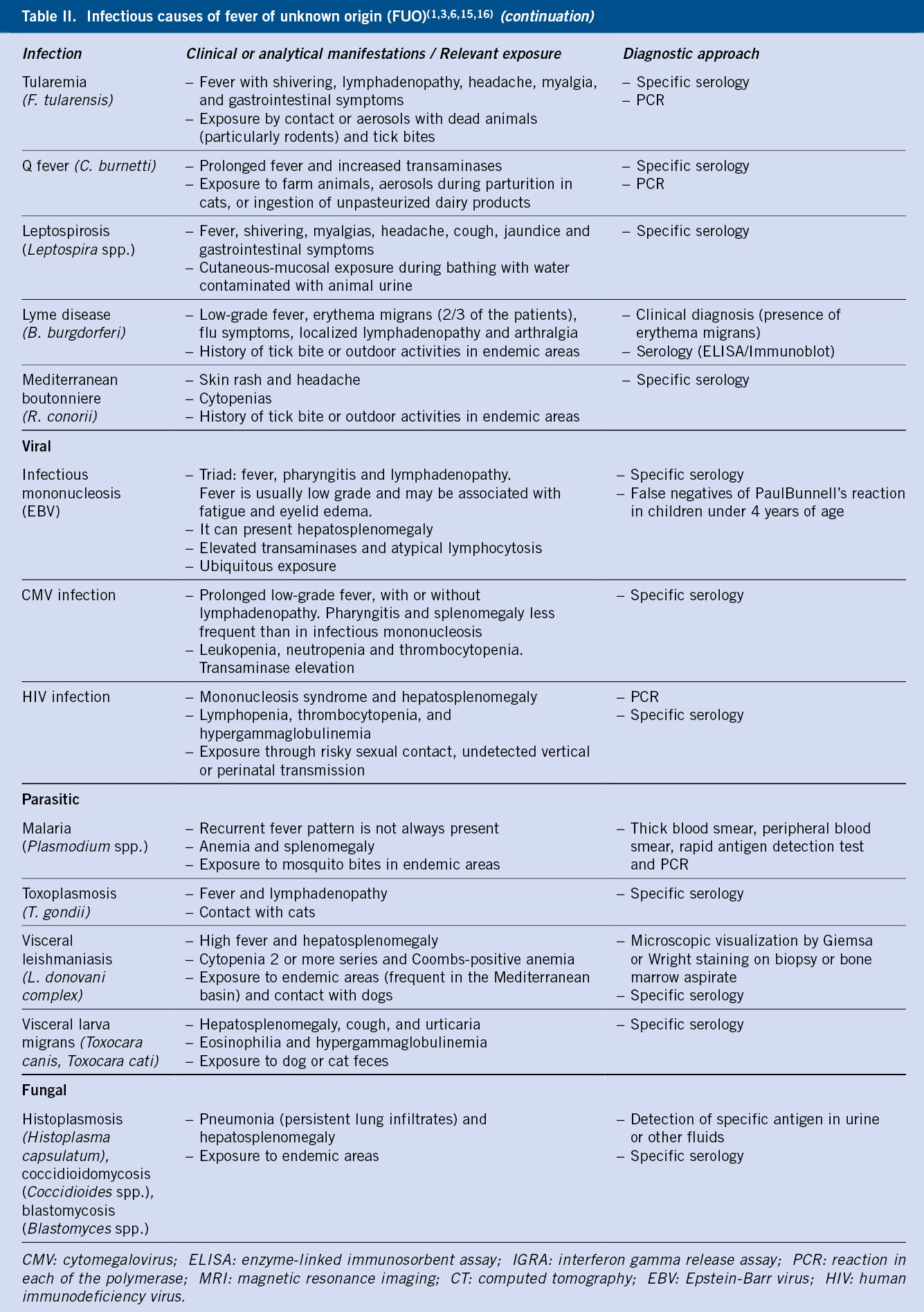
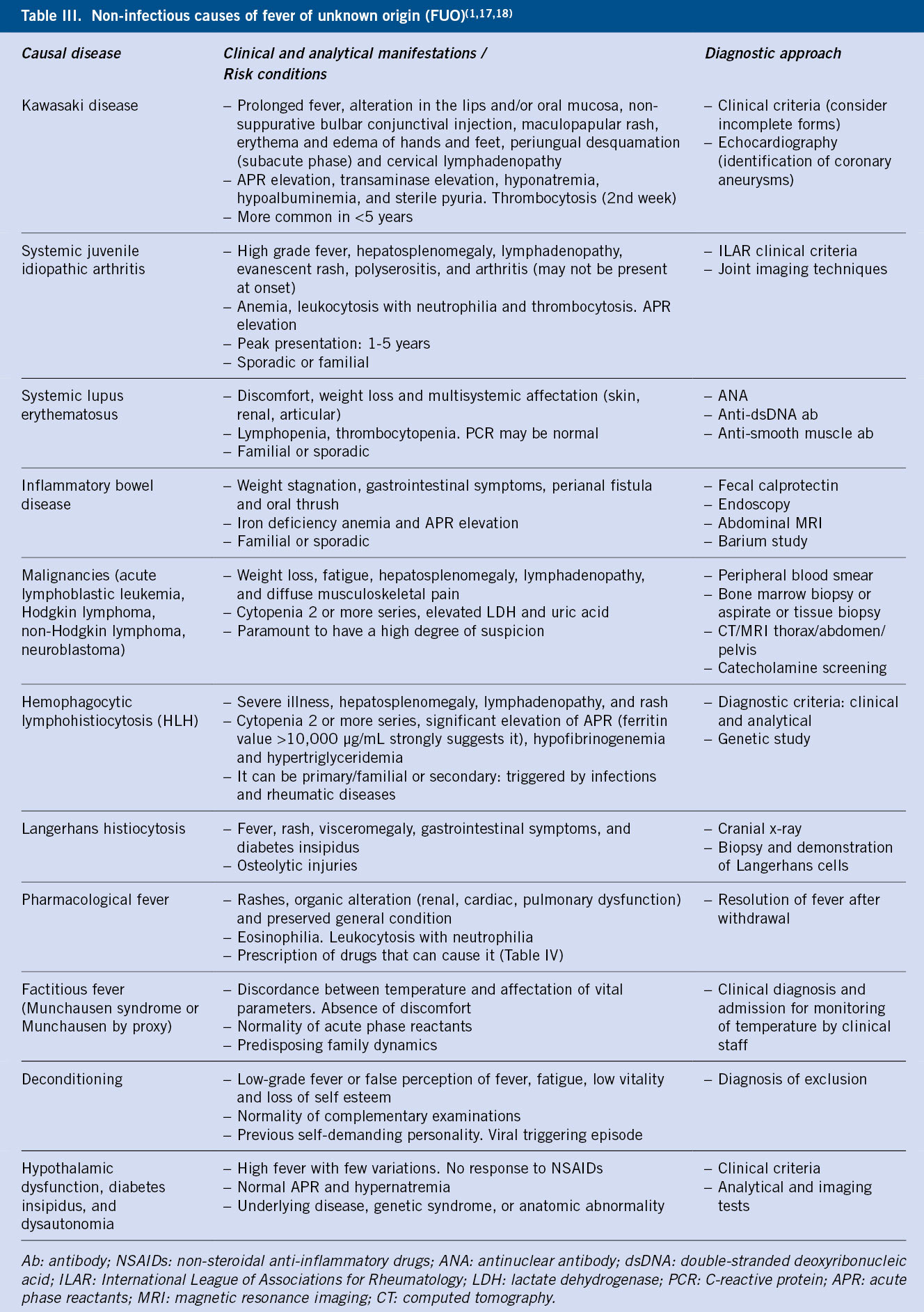
The most frequent cause of FUO in children are infectious diseases, including viral, bacterial and parasitic (Table II). Among the non-infectious causes to consider (Table III), are autoimmune and autoinflammatory diseases, malignant diseases and a variety of other diseases(1).
In a high percentage of cases (in some series almost up to 50%)(4,11), an etiological diagnosis is not reached despite an exhaustive study, this being a predictor of spontaneous resolution without sequelae(1). This high number of undiagnosed cases may be due, in the pediatric population, to more lax inclusion criteria (fewer days of fever) and, in the general population, to a greater availability of better diagnostic techniques (imaging, serological, molecular detection) that allow an earlier diagnosis, before meeting the FUO criteria, meaning that in those cases with real criteria there is a lower probability of reaching a diagnosis(1,3).
In the largest systematic review carried out to date in the pediatric population(12), which included 1,638 patients between 0 and 18 years of age with fever of 1 to 3 weeks duration, the cause was infectious in 51% (of which between 56-71% were bacterial, and 3-15% viral, being the most frequent viral cause in developed countries); the second most frequent situation (23%) was not finding the etiology (more frequent in developed than developing countries, 31% vs 18%), followed by entities included in miscellaneous (11%), autoimmune or autoinflammatory diseases (9%) and, finally, malignant diseases (6%).
In more recent series(9,13), it has been observed that the etiology changes according to the age group and the duration of the fever. Infectious causes are more frequent in children under 6 years of age, with autoimmune diseases and inflammatory bowel disease having a greater relative importance in older children and adolescents(1). Malignant diseases are the least common cause of FUO at all ages. A longer duration of fever reduces the probability of an infectious cause and increases the probability of not reaching a diagnosis(9,14).
Infectious causes (Table II)
Bacterial
Localized infections such as urinary tract infection (especially in children under 2 years of age), pneumonia, sinusitis, mastoiditis, endocarditis or osteoarticular infections (especially those that affect the spine and pelvis due to their difficulty in diagnosis), can be, in paucisymptomatic cases, a cause of prolonged fever, so a high index of diagnostic suspicion must be maintained(2,14).
Abdominal abscesses can also be a cause of FUO. They can occur as a consequence of undiagnosed perforated appendicitis, as a complication of inflammatory bowel disease, previous abdominal surgery, trauma, or pelvic inflammatory disease. We must also consider abscesses in the central nervous system in patients undergoing neurosurgery, as a complication of sinusitis or mastoiditis, or with spinal dysraphisms.
Due to its global incidence, tuberculosis is a diagnosis to be evaluated, especially in patients with suggestive symptoms, compatible radiological findings, exposed to smear-positive cases or who come from areas with a high prevalence. FUO is more common in extrapulmonary and disseminated forms such as miliary(7).
Other microorganisms that cause granulomatous infections should also be considered in case of plausible exposure such as: Bartonella henselae, Salmonella typhi, Brucella spp. and Francisella tularensis. Due to its frequency in our environment, it is important to consider cat scratch disease, even without known close exposure to cats (25% of confirmed cases do not present it)(2,7,15,16). Its most frequent manifestation is localized involvement with adenitis in the drainage lymphatic chain of the inoculation area (where a papule or pustule appears) and that usually resolves without treatment in 2-4 months. Other manifestations may be: FUO, hepatosplenic granulomatous lesions, osteomyelitis, culture-negative endocarditis, and ophthalmic involvement (neuroretinitis and Parinaud’s oculoglandular syndrome). This systemic involvement of the disease requires antibiotic treatment for its resolution, recommending, according to expert opinion, the combination of a macrolide and rifampicin or an aminoglycoside, with a variable duration depending on the involvement and requiring the association of corticosteroids in case of neuroretinitis or severe forms(15,16).
Typhoid fever and brucellosis are common causes of prolonged fever in developing countries, so they should be included in the differential diagnosis in case of travel to these countries or in case of ingestion of unpasteurized dairy products(10).
In case of exposure to wooded areas in endemic regions, various tick-borne diseases such as Lyme disease (Borrelia burgdorferi) or Mediterranean boutonneuse fever (Rickettsia conorii) must be considered. They usually present, in addition to fever, flu-like symptoms, sometimes specific skin disorders and other systemic manifestations(2).
Viral
Viral causes of FUO are mainly due to common childhood viruses that produce symptoms of unusually long duration. Among them, the most frequent are: infectious mononucleosis by Epstein-Barr virus (EBV), and infections by cytomegalovirus (CMV), adenovirus and enterovirus.
Due to its importance, the serological study of the human immunodeficiency virus (HIV) is recommended in all cases, being the cause of prolonged fever in the primary infection (to consider it in adolescent patients) or due to opportunistic infections. A first approximation for its screening is the review of maternal HIV serologies, especially in children without other risk factors, although its negativity does not completely rule out this possibility.
Parasitic
In patients who have traveled in recent months to tropical countries, the diagnosis of malaria should be considered, and it is advisable to request its study in all patients.
Other parasitic causes of FUO to highlight are: toxoplasmosis, leishmaniasis and visceral larva migrans. Toxoplasma gondii infection is the most frequent cause of parasitic infection in temperate climates, and can cause persistent low-grade fever with symptoms similar to infectious mononucleosis. Visceral leishmaniasis, caused by Leishmania donovani complex, is endemic in areas of the Mediterranean coast and is gaining importance in other areas of the Iberian Peninsula; it should be considered in cases of prolonged fever, especially if associated with significant splenomegaly and pancytopenia.
Fungal
The finding of infections by unusual microorganisms (Candida spp., Aspergillus spp. or Cryptococcus spp.) during the study of an FUO should alert us of the possibility of primary or secondary immunodeficiency. We must also suspect immunological defects in infections that do not respond to adequate treatment or that are associated with dermatitis, autoimmune diseases or weight or height stagnation(2,5).
We will consider the diagnosis of endemic mycoses (histoplasmosis, coccidioidomycosis, blastomycosis) in patients with lung disease, if they have previously resided in or traveled to an endemic region. In these cases, we will also assess family occupation, hobbies and leisure activities that may increase their exposure, as well as the presence of birds and bats in the home surroundings(1).
Non-infectious causes (Table III)
Rheumatic diseases
Among the non-infectious causes, the most frequent, in most series, are autoimmune/inflammatory diseases. The most common is the systemic form of systemic juvenile idiopathic arthritis (JIA), followed by systemic lupus erythematosus (SLE) and, more rarely, panarteritis nodosa (PAN). sJIA is a polygenic autoinflammatory disease that should be suspected in patients with high fever spikes, alternating with hypothermia, associated with an evanescent salmon-colored maculopapular rash, more evident during fever spikes, synovial inflammation, polyserositis, lymphadenopathy, hepatosplenomegaly, and elevated of acute phase reactants (APR). Despite requiring the presence of arthritis for its diagnosis, in up to 70% of cases it is not present at its onset(18).
Autoimmune causes must be suspected in the case of prolonged fever with high-grade spikes, especially if it persists despite having empirically initiated broad-spectrum antibiotic treatment(6).
Malignant diseases
Fever in malignant diseases may be due to infection secondary to neutropenia or paraneoplastic phenomena of cytokine release(6). Among the malignant causes of fever, the most frequent are: leukemia, Hodgkin’s lymphoma, and neuroblastoma, which must be actively ruled out, especially if symptoms such as weight loss, poorly defined musculoskeletal pain, night sweats, or adenopathies are associated(2,6).
Miscellaneous
Kawasaki disease is, in developed countries, the most frequent cause of FUO classified as miscellaneous. We must bear this in mind, above all, in incomplete or atypical forms (less than 4 main diagnostic criteria and compatible laboratory and echocardiographic findings) and in children under 6 months of age, in which the manifestation as isolated prolonged fever is more frequent. The diagnosis should be pursued, since the persistence of fever is one of the indications for treatment with intravenous gammaglobulin, beyond the first 10 days of illness(17).
A recently described entity with common clinical features is multisystem inflammatory syndrome in children (MIS-C), a rare complication following SARS-CoV-2 infection. It usually presents with prolonged fever associated with signs and symptoms of cardiovascular, mucocutaneous and/or gastrointestinal involvement.
In inflammatory bowel disease, fever may become more important than abdominal symptoms, especially in Crohn’s disease. Its active search should be carried out in cases of elevated APR, anemia, weight loss or failure to thrive, even without gastrointestinal symptoms.
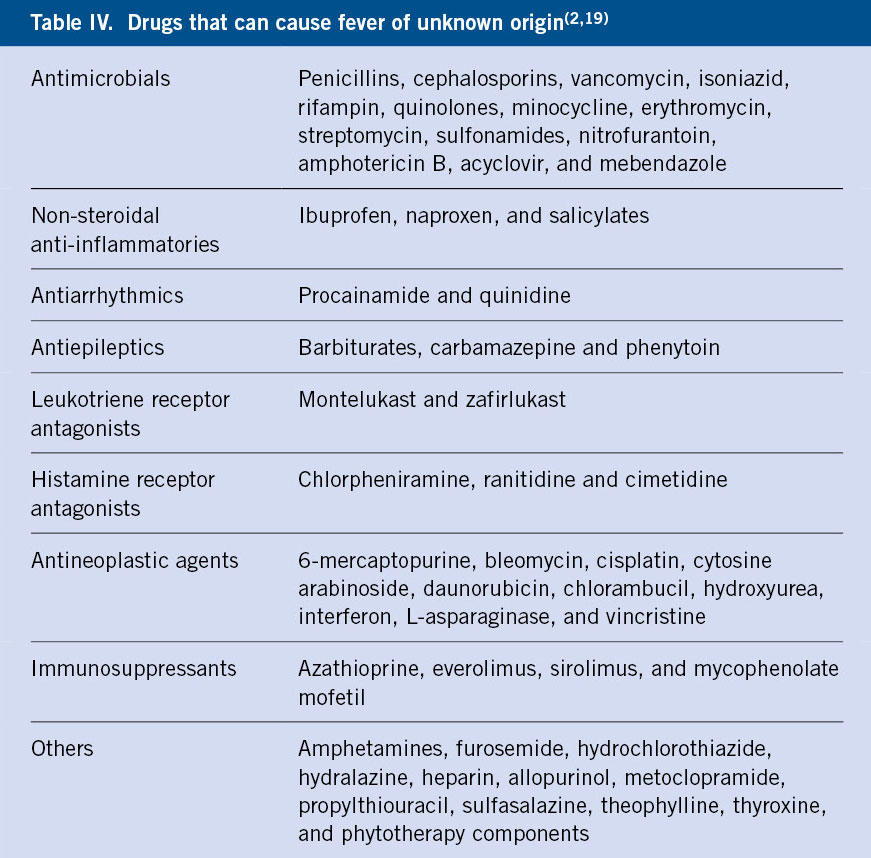
Fever is a common adverse drug reaction. Although it has been described more commonly in association with certain drugs (Table IV), it can potentially be attributed to practically any drug. It is important to also take phytotherapy products or unconventional therapies into account during the medication history. Drug-caused fever usually resolves in the first 48-72 hours after its withdrawal, so it is recommended that any non-essential medication should be withdrawn at the start of the FUO study(2,18).
An entity called deconditioning has been described in adolescents, which usually occurs after a well-defined febrile episode. It is characterized by low-grade fever or erroneously perceived as fever associated with fatigue and decreased vitality. This discomfort usually causes the inability to go to school continuously and carry out activities that, prior to the onset of the clinical picture, were performed normally. There is usually some discrepancy between the number and severity of the symptoms reported and the normality of the physical examination and complementary tests(1,3).
Lastly, and as a diagnosis of exclusion, we must consider factitious fever. It is that fever simulated by the patient (Munchausen syndrome) or by the parents/caregivers (Munchausen syndrome by proxy). It should be suspected in cases of fever with an unusual pattern (very brief peaks or no evening increase in temperature), absence of tachycardia with fever or warmth to the touch, as well as non-detection of fever by another observer(3).
Diagnosis
The evaluation of patients with fever of unknown origin should always begin with a thorough clinical history and physical examination. Their findings will guide us to the complementary tests, which will be requested in stages.
History
In the history, questions will be asked about the fever (duration, degree, method of measurement, frequency, pattern and response to antipyretics), as well as each of the associated symptoms and signs (rash, oral thrush, gastrointestinal symptoms, weight loss, arthralgia, etc.), recording its temporal relationship with fever. The demonstration of the presence of fever in a medical environment is a critical point before continuing with the study. In the case of outpatient care, the family will be asked to keep a fever diary, recording at least two temperature measurements at the ends of the day, always at the same time and with the same method(5).
The following should be inquired: the patient’s medical history, including the vaccination status, weight-and-height (weight and height curves should be plotted) and psychomotor/neurocognitive progression; epidemiological context, including international travel history and prophylactic measures; and exposure to people with contagious infections, to animals, insect bites, or food consumption that may pose a risk. The medical history should be recorded, including previous admissions and surgeries, as well as any drugs or other medicinal products that the patient may be receiving. In adolescents, we must ask about sexual activity that could expose them to a risk of infections through this route(5,7). We will actively inquire about family history of autoimmune disease, immunodeficiency or recurrent or unusual infections.
If a diagnosis is not reached, it is essential to periodically re-interrogate, trying to find information that has been forgotten or considered of little importance in previous anamnesis.
Physical examination
Physical examination must be complete and structured through systems, including(3,7,14):
• Vital parameters: assess the adequate increase in heart rate with fever (heart rate increases around 10 beats per minute for every 1ºC of body temperature above normal temperature)(20).
• General: weight-height evaluation and comparison with previous measurements given the possibility of weight loss or decreased growth in the context of to the episode.
• Skin: maculopapular rashes can be found, guiding towards viral pictures or Kawasaki disease; evanescent salmon-like rash associated with fever in systemic JIA; petechiae in other viral infections or infective endocarditis; lesions such as chronic erythema migrans, which suggests Lyme disease; or lesions compatible with other insect bites, including ticks, that can indicate vector-borne diseases.
• Oral and pharyngeal mucoses: presence of pharyngeal hyperemia with or without exudates; oral thrush; or other abnormalities of the oral mucosa, such as raspberry tongue or cracked lips.
• Cardio-respiratory: the presence of murmurs or abnormality of heart tones should be evaluated. Abnormalities in the respiratory auscultation or presence of clubbing should be detected.
• Reticuloendothelial: examination of the lymph nodes of all palpable territories (occipital, pre and retroauricular, cervical, supraclavicular, axillary, epitrochlear, inguinal and popliteal) and a record and description of its characteristics. Palpation of hepato or splenomegaly in infections or other diseases that may cause them.
• Ophthalmic: Assess the presence of conjunctivitis with or without discharge, eyelid edema, signs of uveitis, and involvement of the fundus.
• Gastrointestinal: Abdominal examination for signs of localized pain or peritonism suggestive of abscesses, or the presence of visceromegaly. We will evaluate the presence of fissures or rectal fistulas.
• Musculoskeletal: Bone palpation for tender points and inspection of all joints for asymmetries, phlogotic signs, or impaired range of motion.
• Genital/Gynecologic: In adolescents, look for signs of sexually transmitted infections or genital thrush.
Tables II and III show the most frequent signs on examination of some entities that are included in the differential diagnosis of FUO.
The physical examination should be repeated daily if the patient is hospitalized, preferably during fever in order to assess possible clinical signs absent in apyrexia; or, in each of the visits, if the follow-up is carried out on an outpatient basis.
An incomplete clinical history or physical examination, which causes a delay in the diagnosis or in the request for complementary tests that lead to it, can be a cause of persistence of fever, to be avoided(7).
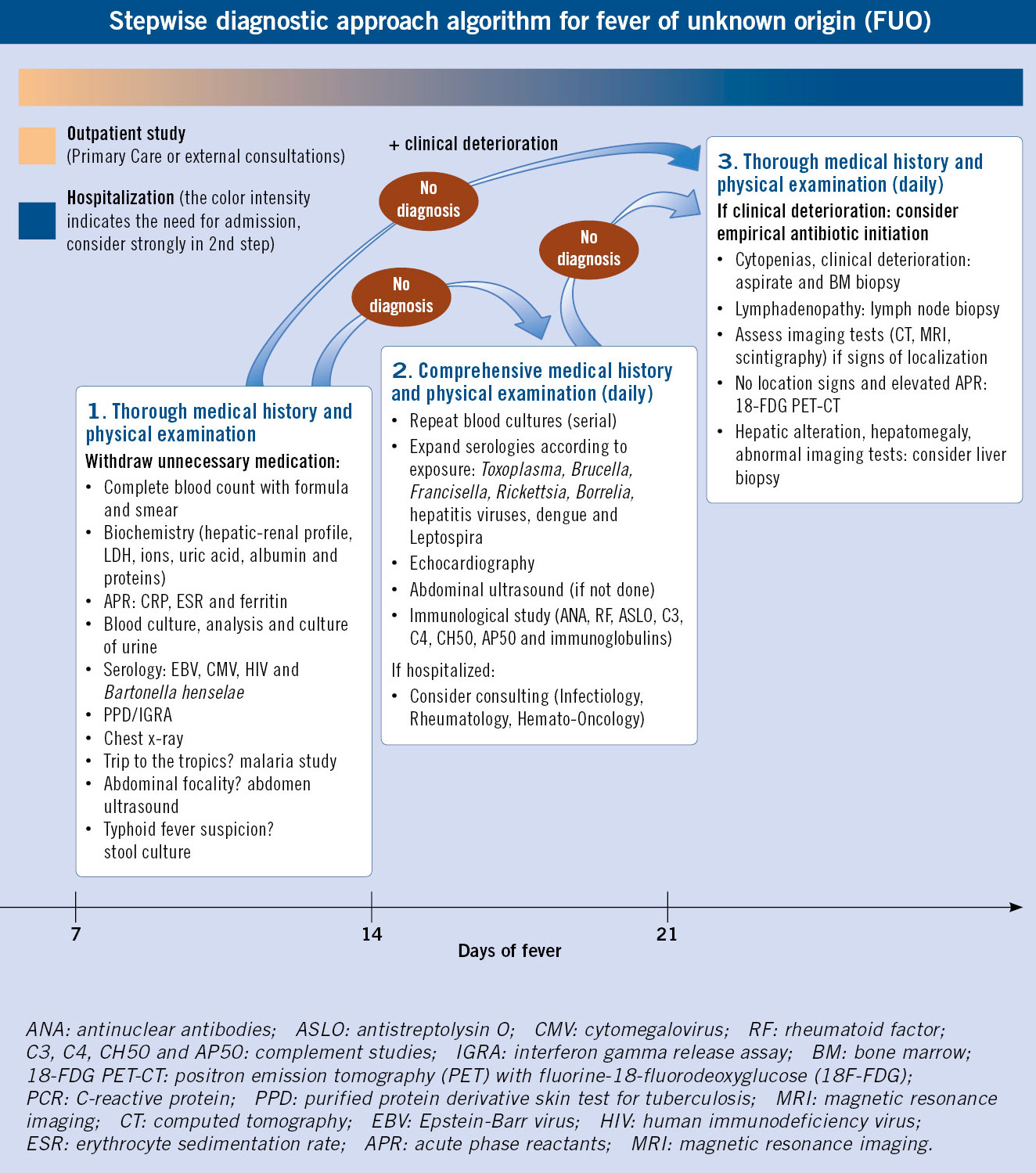
Complementary tests
The FUO diagnostic process is carried out in stages in various phases, guided by the data obtained from the history and physical examination, trying to initially rule out those diseases that, due to age, frequency in our environment or history of exposure, are more plausible (Algorithm). Its objective is to arrive at an early diagnosis, avoiding unnecessary tests and ensuring a rational use of resources. Despite the fact that various diagnostic algorithms have been proposed(2,3,5,7,21), no studies have been carried out that demonstrate the superiority of one over the other for early detection of the cause of FUO in pediatric patients.
The speed at which the study will progress will depend on the clinical status of the patient and the presence or absence of findings in previous phases, reserving the most invasive tests for cases suggestive of severe disease(1,5).
We must remember the importance of repeating the clinical history and physical examination at each of the steps, in search of new details or clinical findings that allow us to direct and optimize our requests, avoiding unnecessary tests.
Complementary tests that are recommended in the first step for most patients with FUO include: complete blood count with formula, peripheral blood smear, basic biochemistry (liver and renal profile, lactate dehydrogenase [LDH], ions, uric acid, albumin and total proteins), acute phase reactants (C-reactive protein [CRP], erythrocyte sedimentation rate [ESR] and ferritin), blood culture, urinalysis and urine culture, tuberculin skin test and/or interferon gamma release test (IGRA) and chest X-ray (even without respiratory symptoms)(1). The first step also includes Epstein-Barr virus, cytomegalovirus and B. henselae serologies, given their high frequency, and HIV due to its importance. This first phase should also include, if they are compatible with the history and the initial examination: other microbiological studies such as the study of malaria (in the case of history of travel to an endemic area) or stool culture, if typhoid fever is suspected; and serological studies included in the second step or imaging, such as an abdominal ultrasound, if associated with abdominal symptoms or elevated liver enzymes in the laboratory tests.
In a second step, repeating blood cultures if the previous ones are negative is recommended, as well as to expand the serological study according to the clinical history, including: T. gondii (contact with cats), Brucella spp. (unpasteurized milk intake), F. tularensis (rodent exposure), Rickettsia spp. or Borrelia spp. (tick bite), etc., if they have not been done previously. An echocardiography is also recommended to evaluate the coronary arteries and the presence of vegetations, as well as an abdominal ultrasound if it had not been requested in the first phase. If there are suggestive symptoms, it is advisable to perform a sinus CT, since sinusitis is a relatively common cause of FUO(5). If there are no localization signs, other imaging tests are not recommended (computerized tomography, magnetic resonance imaging or scintigraphy), as they present very low diagnostic yield(9,10). In children with suggestive findings, especially those over 5 years of age, an immunological study will be requested that includes: rheumatoid factor (RF), antinuclear antibodies (ANA), antistreptolysin O (ASLO), complement (C3, C4, CH50 and AP50) and determination of immunoglobulins. During this second phase, if this possibility is available, it is advisable to consult pediatricians specializing in Infectious Diseases, Rheumatology and/or Hematology and Oncology, depending on the suspicion.
If the diagnosis is not achieved at this point, a third step will be accessed including more invasive methods, also based on clinical findings: lymph node biopsy in case of lymphadenopathy; liver biopsy, if abnormality in ultrasound or involvement of the liver function tests in the blood; or aspirate or biopsy of bone marrow, if alterations are observed in peripheral blood. Bone marrow examination must be performed earlier in the case of severe patients or with progressive clinical deterioration, to rule out lymphoproliferative processes, hemophagocytic lymphohistocytosis (HLH) or establish the diagnosis of visceral leishmaniasis(10). Screening for endocrinological pathologies, without clear suspicion, does not usually give results, so it is not generally recommended(1).
In this last step, the performance of a PET-CT with 18-FDG can be considered, which can help in the detection and differentiation of infectious, inflammatory and malignant causes. A retrospective study with 110 pediatric patients showed that it could detect the cause of fever in about half of the cases, in which it had not been detected with the previously performed tests. The positive predictive value of up to 84.1% was positively associated with elevated CRP. In addition, if no abnormalities were found, it showed a high predictive value for spontaneous resolution of fever(21).
Admission criteria
The FUO study can be performed, in most patients, on an outpatient basis, provided their general condition allows it, with visits at frequent intervals that allow us to perform a recapitulation of the clinical history and a complete physical examination at each visit. If fever persists and no cause has been found, diagnostic tests will be performed in successive phases and hospital admission is recommended at that stage(1). At any time, in the event of localization signs, clinical worsening with progression of symptoms, or abnormalities in the tests performed that require close observation or in order to speed up the diagnostic process, hospital admission will also be indicated. Other admission indications are to ensure the presence of fever and to determine its pattern in cases where there are uncertainties about its correct measurement at home or when it has not been confirmed in the ambulatory visits.
Treatment
Empirical treatment should be avoided in stable patients and without a specific diagnostic suspicion, since it could delay the diagnosis.
The withdrawal of medication or products that may cause fever for diagnostic-therapeutic purposes is one of the first steps to be taken. A gradual withdrawal is recommended in case of receiving various drugs, to identify the causative agent(3,9).
In case of clinical stability, symptomatic treatment will be carried out until the etiology is clarified, followed by targeted treatment if necessary. The empirical use of antibiotics or corticosteroids is not recommended, as they could delay or mask the diagnosis(5,7,10,14). The exceptions are: suspicion of miliary tuberculosis (antituberculosis drugs indicated), high suspicion of JIAs (non-steroidal anti-inflammatory drugs, glucocorticoids) or Kawasaki disease (treatment with intravenous immunoglobulin infusion and acetylsalicylic acid). Only in case of clinical deterioration during the diagnostic process with suspicion of serious bacterial infection, the initiation of antibiotic treatment of a spectrum appropriate to the diagnostic suspicion would be indicated.
Prognosis
Variable prognosis depending on the etiology, generally good, if a diagnosis is not reached.
The prognosis will largely depend on the etiology of FUO. In cases in which a diagnosis is not reached after an adequate study, the long-term prognosis is good, with resolution of symptoms and absence of sequelae in most cases.
Conclusions
Fever of unknown origin (FUO) is, in most pediatric cases, a benign and/or self-limiting process.
It is important to differentiate, early, benign causes from those that may be a manifestation of a severe condition or that may pose a vital risk.
Initial evaluation of FUO requires confirmation of fever in a medical setting and careful reassessment of the history and physical examination.
The majority are due to infectious causes, but a non-negligible percentage is due to other causes, including rheumatic or neoplastic diseases.
In a high percentage of cases an etiological diagnosis is not reached, being a marker of spontaneous resolution.
Complementary tests should be carried out in stages and always guided by the findings of the clinical history and physical examination to improve their profitability.
Empirical antibiotic or anti-inflammatory treatment is not recommended if the patient presents clinical stability, except in selected cases, since it could delay the diagnosis.
Role of the Primary Care pediatrician
The Primary Care pediatrician, as a reference figure in child health for most families, will receive a large part of the consultations for prolonged fever, so it is important to have an adequate initial assessment.
A detailed history and physical examination (with temperature determination in the office) will be the initial step in this evaluation.
In clinically stable cases, close follow-up for reassessment of the patient and the recommendation to carry out a calendar of fever and associated symptoms/signs will allow additional information to be obtained on the evolution of the clinical picture. The knowledge of the family, acquired over the years, can also make it possible to recommend or discourage this home observation.
This approach should allow the distinction of the fever pattern presented by the patient. In the event of considering FUO, the primary care pediatrician can guide the suspected diagnosis and, if considered appropriate, continue the study by requesting first-level complementary tests. The difficulty at this stage is to early differentiate the benign causes of FUO from those that may pose a vital risk.
Referral to hospital care will be indicated in the event of clinical worsening, persistence of fever without diagnosis after first-level tests (with the need to expand the study with tests not usually available from Primary Care), or abnormalities in the tests performed that require an inpatient observation and/or expedite the diagnostic process.
Conflict of interest
There is no conflict of interest in the preparation of the manuscript. Declaration of interests: none.
Bibliography
The asterisks show the interest of the article in the opinion of the authors.
1.*** Manthiram K, Edwards KM, Long SS. Prolonged, Recurrent, and Periodic Fever Syndromes. In: Long SS, Prober CG, Fischer M, Kimberlin DW. Principles and Practice of Pediatric Infectious Diseases. 6th ed. Philadelphia: Elsevier; 2023. p. 123-34.
2.** Rigante D, Esposito S. A roadmap for fever of unknown origin in children. Int J Immunopathol Pharmacol. 2013; 26: 315-26. Available in: https://doi.org/10.1177/039463201302600205.
3.** Ruiz-Contreras J, Durán-Lorenzo I. Fiebre de origen desconocido en niños. Fever of unknown origin in children. Pediatr Integral. 2018; XXIII: 229-35. Available in: https://www.pediatriaintegral.es/publicacion-2018-07/fiebre-de-origen-desconocido-en-ninos/.
4. Marshall GS. Prolonged and recurrent fevers in children. J Infect. 2014; 68: S83-S93. Available in: https://doi.org/10.1016/j.jinf.2013.09.017.
5.** Chusid MJ. Fever of Unknown Origin in Childhood. Pediatric Clin North Am. 2017; 64: 205-30. Available in: https://dx.doi.org/10.1016/j.pcl.2016.08.014.
6.*** Reynolds S. Kadambari S, Calton E, Roland D. The child with prolonged fever: when to think zebras. Pediatrics and Child Health. 2020; 30: 261-9. Available in: https://doi.org/10.1016/j.paed.2020.04.004.
7. Escosa-García L, Baquero-Artigao F, Méndez-Echevarría A. Fiebre de origen desconocido. Fever of unknown origin. Pediatr Integral. 2014; XVIII: 15-21. Available in: https://www.pediatriaintegral.es/numeros-anteriores/publicacion-2014-01/fiebre-de-origen-desconocido/.
8.** Petersdorf RG, Beeson PB. Fever of unexplained origin: report on 100 cases. Medicine (Baltim). 1961; 40: 1-30. Available in: https://doi.org/10.1097/00005792-196102000-00001.
9.** Antoon JW, Peritz DC, Parsons MR, Skinner AC, Lohr JA. Etiology and resource use of fever of unknown origin in hospitalized children. Pediatric Hosp. 2018; 8: 135-40. Available in: https://doi.org/10.1542/hpeds.2017-0098.
10. Ramos-Amador JT, Álvarez-García A, Ruiz-Jiménez M. Fiebre de origen desconocido en Pediatría. Fever of unknown origin in Pediatrics. In: Mellado-Peña MJ, Calvo-Rey C, Rojo-Conejo P. Infectología pediátrica básica: manejo práctico. Sociedad Española de Infectología Pediátrica. Madrid: Editorial Panamericana; 2012. p. 15-22.
11. Statler VA, Marshall GS. Characteristics of patients referred to a pediatric infectious diseases clinic with unexplained fever. J Pediatric Infect Dis Soc. 2016; 5: 249-56. Available in: https://doi.org/10.1093/jpids/piv008.
12.*** Chow A, Robinson JL. Fever of unknown origin in children: a systematic review. World J Pediatric. 2011; 7: 5-10. Available in: https://doi.org/10.1007/s12519-011-0240-5.
13. Szymanski AM, Clifford H. Ronis T. Fever of unknown origin: a retrospective review of pediatric patients from an urban, tertiary care center in Washington, DC. World J Pediatric. 2020; 16: 177-84. Available in: https://doi.org/10.1007/s12519-019-00237-3.
14. Hernández Bou S. Fiebre prolongada. Prolonged fever. In: Garcia JJ, Cruz Martinez O, Mintegi Raso S, Moreno Villares JM. Cruz Manual of Pediatrics. 4th ed. Madrid: Ergon; 2020. p. 108-12.
15. Zangwill KM. Cat Scratch Disease and Bartonellaceae: The Known, the Unknown and the Curious PIDJ. 2021; 40: S11-5.
16. Han JY, Vijayan V. Bartonella Species (Cat-Scratch Disease). In: Long SS, Prober CG, Fischer M, Kimberlin DW. Principles and Practice of Pediatric Infectious Diseases. 6th ed. Philadelphia: Elsevier; 2023. p. 901-5.
17. Barrios-Tascón A, Centeno-Malfaz F, Rojo-Sombreo H, Fernández Cooke E, Sánchez-Manubens J, Pérez-Lescure Picarzo J. Consenso nacional sobre diagnóstico, tratamiento y seguimiento cardiológico de la enfermedad de Kawasaki. National consensus on diagnosis, treatment, and cardiology follow-up of Kawasaki disease. An Pediatr (Barc). 2018; 89: 188. e1-e22. Available in: https://doi.org/10.1016/j.anpedi.2018.04.003.
18. Mosquera-Angarita JM. Systemic juvenile idiopathic arthritis. Protoc diagn ter pediatr. 2020; 2: 61-75.
19. Patel RA, Gallagher FC. Drug Fever. Pharmacotherapy 2010; 30: 57-69. Available in: https://doi.org/10.1592/phco.30.1.57.
20. Daymont C, Bonafide CP, Brady PW. Heart Rates in Hospitalized Children by Age and Body Temperature. Pediatrics. 2015; 135: 1173-81. Available in: https://doi.org/10.1542/peds.2014-3738.
21.** Pijl JP, Kwee TC, Legger GE, Peters HJ, Armbrust W, Schölvinck EH. Role of FDG-PET/CT in children with fever of unknown origin. Eur J Nucl Med Mol Imaging. 2020; 47: 1596-604. Available in: https://doi.org/10.1007/s00259-020-04707-z.
Recommended bibliography
– Manthiram K, Edwards KM, Long SS. Prolonged, Recurrent, and Periodic Fever Syndromes. In: Long SS, Prober CG, Fischer M, Kimberlin DW. Principles and Practice of Pediatric Infectious Diseases. 6th ed. Philadelphia: Elsevier; 2023. p. 123-34.
Excellent review chapter on prolonged and recurrent fever and periodic fever syndromes in one of the reference manuals in pediatric infectious diseases. It includes definitions of the different fever patterns, as well as a broad differential diagnosis based predominantly on infectious causes of FUO and its diagnostic approach.
– Chow A, Robinson JL. Fever of unknown origin in children: a systematic review. World J Pediatric. 2011; 7: 5-10. Available in: https://doi.org/10.1007/s12519-011-0240-5.
The largest systematic review published to date, by number of studies and patients included, on the causes of FUO. It includes studies conducted in developed and developing countries.
– Reynolds S. Kadambari S, Calton E, Roland D. The child with prolonged fever: when to think zebras. Pediatrics and Child Health. 2020; 30: 261-9. Available in: https://doi.org/10.1016/j.paed.2020.04.004.
This article addresses when to consider, in patients with prolonged fever, the less common infectious, autoimmune, or malignant causes and their diagnostic-therapeutic approach.
| Clinical case |
|
A 6-year-old girl, previously healthy, is assessed by her pediatrician because of fever lasting 12 days (maximum 38.5ºC), associated with general malaise during temperature rise and fatigue. They have attended for evaluation by the pediatrician on 2 occasions. Given the absence of abnormalities in the physical examination, the general condition preserved in fever-free intervals and laboratory tests including a normal complete blood count and general biochemistry, carried out on the fourth day of fever, he had decided to carry out clinical follow-up, asking the parents to keep a fever diary. Since the last visit, the mother reports increased loss of appetite that has caused her weight loss and abdominal discomfort, without vomiting or diarrhea. The presence of fever, predominantly in the evening, with 2-3 daily peaks and with adequate response to antipyretics, is confirmed with the diary. She has not presented rashes since the onset of the fever. The family is inquired on the history of fever again. The patient has no pathological history of interest or drug allergies. The growth curve is reviewed, showing a good weight-height development. She has received all the vaccinations included in the schedule. She has a healthy older brother and they do not report relevant diseases in the family. They live in an urban environment with a dog and have not traveled in the last year. On physical examination, she was febrile (38.2ºC), well hydrated, with normal color, and with good skin perfusion. She presented a 3 mm papular lesion on the right forearm with no signs of superinfection, without skin rash. Lymphadenopathy was not palpable. Cardiorespiratory auscultation showed no abnormalities, no murmurs were heard. The abdomen was soft with slight pain on palpation in both hypochondria, with a slight palpable hepatosplenomegaly, both organs palpated about 2 cm below the costal margin. Given the persistence of the fever, confirmed at the visit and through the diary, and the appearance of gastrointestinal symptoms with hepatosplenomegaly on examination, it was decided to refer the patient to the Emergency Department for additional tests and admission to allow close and careful observation as well as to complete the study. On arrival at the ER, she was already afebrile, with an unchanged physical examination. She is contemplated as fever of unknown origin, and the following complementary tests are requested: • Blood analysis with complete blood count and biochemistry: Hb: 12.5 g/dl; 10,500/mm3 leukocytes (neutrophils 6,800/mm3, lymphocytes 2,500/mm3); CRP: 7.5 mg/dl, ESR: 52 mm/h; renal and hepatic function show no alterations. • Unaltered urine analysis. • Blood culture: pending results. • Stool culture (given the presence of gastrointestinal symptoms): pending results. • Serological study: Epstein-Barr virus, cytomegalovirus, HIV, adenovirus: results pending. • Chest X-ray: shows no abnormalities. • An abdominal ultrasound was also requested, in which no signs of appendicitis or free fluid were observed, mild hepatosplenomegaly was confirmed with multiple small hypoechoic lesions in the liver and spleen, and mesenteric lymphadenopathies.
|
 Fever of unknown origin
Fever of unknown origin