|
| Topics on Continuous Training |
M.I. Hidalgo Vicario*, L. Rodríguez Molinero**
*Pediatrician. Doctor in medicine. Accredited in Adolescent Medicine. Former president of the SEMA. Madrid. **Pediatrician. Doctor in medicine. Accredited in Adolescent Medicine. La Marquesina Medical Center. Valladolid
| Abstract
The stage of adolescence becomes socially relevant in industrialized countries after World War II and is linked to social progress more than any other stage of life. In industrial and consumer societies there is great interest in studying and understanding the events that take place in adolescence, from physical to mental and social changes. Adolescents suffer from diverse pathologies, many of which are related to their risk behaviors. There has been a switch in relation to chronic diseases due to medical advances, whereby infant mortality has been reduced and thus, life expectancy increased, even into adulthood. The main causes of death are preventable. All the pathologies and risk factors avoided or corrected during this period will lead to healthier adults in the future. The difficulties and care failures that occur when the adolescent grows up and starts to be looked after by other professionals have been verified. Guidelines and protocols to facilitate the process of transitioning care from the pediatrician to the adult physician are suggested. Strategies to improve the health of adolescents proposed by various international organizations are also presented. |
| Resumen
La etapa de la adolescencia toma relevancia social en los países industrializados a partir de la II Guerra Mundial y está ligada a la evolución social más que ninguna otra etapa de la vida. En las sociedades industriales y de consumo, existe mucho interés por estudiar y comprender lo que sucede en la adolescencia, desde los cambios físicos a los mentales y sociales. Los adolescentes sufren diferentes patologías y muchas están relacionadas con sus conductas de riesgo. Debido a los avances médicos, se ha visto un cambio en relación a las enfermedades crónicas, en las que se ha reducido la mortalidad infantil, incrementado la esperanza de vida, incluso hasta la edad adulta. Las principales causas de muerte son evitables. Todas las patologías y factores de riesgo que se eviten o corrijan durante este periodo, servirán para tener unos adultos más sanos en el futuro. Se han constatado las dificultades y los fallos asistenciales que se producen cuando el adolescente crece y pasa a ser atendido por otros profesionales. Se sugieren pautas y protocolos para facilitar el proceso de transición del cuidado del pediatra al médico de adultos. Diferentes organismos internacionales proponen estrategias para mejorar la salud de los adolescentes. |
Key words: Adolescent; Adolescent epidemiology; Adolescent health; Care transition.
Palabras clave: Adolescente; Epidemiología del adolescente; Salud del adolescente; Transición del cuidado.
Pediatr Integral 2022; XXVI (4): 200 – 213
OBJECTIVES
• To update the knowledge about adolescence nowadays. The concept of adolescence as a social phenomenon changes with ideologies, values, care plans and demographic data.
• To define which theories are more powerful in terms of understanding the psychology of adolescents and their
behaviors.
• To analyze the epidemiological situation worldwide and in Spain: mortality, morbidity, reasons for consultation and causes of hospital admission.
• To understand why the health of adolescents deteriorates and how their health assistance is provided in our country.
• To know how “the transition” process from the various care levels should be carried out to achieve higher efficiency.
• To describe the strategies of world organizations to deal with “adolescence as an age of risk”.
Adolescence. Epidemiological situation. Most frequent pathology. Transition
Introduction
The stage of adolescence takes on social relevance in industrialized countries after World War II and is linked to social evolution more than any other stage of life.
The RAE Dictionary (Royal Academy of Spanish language) defines adolescence as the stage between childhood and adulthood. Etymologically, it comes from adolescere and its present participle adolescens, which means growing and developing. This definition encompasses the two most decisive characteristics of this stage: growth and development.
The division of life into ages comes from ancient times. Already in the Corpus Hipocraticum, the different stages of life mentioned: infancy, childhood, youth, adulthood and old age. The limits are imprecise. Charlotte Bühler in the 19th century, admitted that there were some critical stages in life, when it is not about chronological age, but about the way to carry out that “step”. That would be the first concept of adolescence, as we understand it today.
The stage of adolescence takes on social relevance in industrialized countries after World War II. The economic, sociological and cultural changes conditioned the delay of the incorporation of the adolescent to adult life. At the same time, the advancement of biological phenomena progressively increases this imbalance. The emergence of competitiveness, consumption, and welfare society have contributed to the raise of problems, previously unknown.
Adolescence is linked to social progress more than any other stage of life. When life expectancy was short, adolescents were the successors of the family, they had to assume responsibility early on. They were a cheap, docile and efficient workforce. They were traditionally used for military purposes. They have oftentimes been the object of abduction by ideological groups, sects, minorities… In no other stage of existence does social life influence so much as in this one, and the example that best demonstrates this, is the influence of temporary fashions and how much they are suffering in the current COVID pandemic, with the significant increase in psychological problems and suicide attempts.
There are many ways to “get through” adolescence. That is why we speak of “adolescences”. However, we are still far from achieving a society tailored to adolescents. Until there is a stable and balanced economy, educational plans made for each group of adolescents, communicative family dynamics and adequate health care, adolescence will continue to exist as a social risk group.
In our traditions there are numerous examples of rites, festivals or ceremonies for the passage from childhood to a mature age, which differ based on the meaning that adolescence had in each period of time.
In our western culture, we find traditional stories that try to clarify the mysteries of the cycles of life, for example, in classical mythology. Classical myths represent the events that take place in adolescence, as if the historical unconscious anticipated what has subsequently been analyzed in a more scientific way. In this sense, there are numerous myths, such as: Adonis (“an extremely attractive young man, often also vain”), Persephone (“an innocent maiden, a mother’s sorrow for the kidnapping of her daughter and the joy at her return; the explanation of natural processes, with the departure and return of the goddess causing the change of season”), Artemis (“virginity; the goddess who brought and also relieved women’s diseases”), Aphrodite (“goddess of beauty, sensuality and erotic love”), Narcissus (“unable to love another person because he loved himself too much”) or Cupid (“god of love and desire”). Could it be considered that these aspects are consubstantial with the life course of men? Isn’t adolescence the concentration of all those vicissitudes of the human being?(1).
Adolescence begins with puberty and has an indeterminate end, as this has been prolonged in recent years due to the greater time that the young person invests in his/her training. There is no consensus among authors about the ages it comprises. The World Health Organization (WHO) places it between 10 and 19 years, although some organizations, such as the American Pediatric Association, consider that this period extends to 21 years of age. Given that it is a stage of development and that it extends around 10 years, it seems obvious to think that there will be differences throughout its course, which is why three stages have been defined, that overlap each other: up to 13 years, the early adolescence; from 14 to 17, middle adolescence; and from 18 to 21 years of age, late adolescence. This classification is illustrative and relative, as it varies with ethnicities, cultures and geographical location.
Adolescence is, therefore, a stage of rapid, extensive, very significant and determining changes. It is an evolutionary crisis with constant personal, family, academic and social adaptations and readaptations. Culturally, it develops into an “unlimited” consumption offer, with a loss of the educational and protective role of parents; on many occasions, with uncertain future horizons, in a society that overstimulates and excites the population and that, on many occasions, denies education and assistance (López, 1999). Adolescence, as a social phenomenon, is not analyzed from the point of view of physiological changes, but by its evolutionary psychological traits, its search for identity, its desire to find a place in the world and the influence of trending fashions and values. The western world of consumption, industry, marketing and production, create traps and generates frustrations and hopelessness for which, biologically, adolescents are less prepared(1).
Theories about adolescence
In industrial and consumer societies there is much interest in studying and understanding what happens in adolescence, from physical to mental and social changes.
In the mid-nineteenth century, Psychology rose as an autonomous discipline. Later, Child Psychology appeared in Germany, Comparative Psychology in England and Adolescent Psychology in the USA. Relevant authors who have been concerned with the study of adolescence include: Stanley Hall, Gesell, Freud (psychosexual development), Rank, Sullivan, Erikson, Blos, Spranger, Piaget (cognitive structures), Remplein (structural synthesis), Lewin (typological theory), Malinosky, Margaret Mead (Anthropology), Bandura (social learning), etc.
In industrial and consumer societies there is much interest in studying and understanding what happens in adolescence, from physical to mental and social changes. There are many ways to explain everything that happens at this stage. We are going to focus on those theories that have had the greatest diffusion and influence(2).
Psychoanalytic approach
The changing body of the adolescent is subject to conflicting emotions that generate confusion. There is a tension between the body and the mind that takes time to understand. The young child who wants to be attended and cared for becomes the adolescent who claims his space and the right to decide, sometimes showing contempt for his parents. These situations are related to psychological functioning. Some authors emphasize the evolution of the child’s sexuality in transition to adulthood and others point to, as a priority, the mourning that occurs due to past childhood.
Cognitive-evolutionary approach. Piaget’s theory
Adolescence is seen as a transition period in which important cognitive changes occur. Fundamentally, formal thinking is accessed (solving difficulties and reasoning functions). According to Piaget, adolescents reach the highest level of cognitive development (formal operations), when they reach the capacity to produce abstract thought. It gives them new and more flexible ways to use information. The ability to produce abstract thought has emotional implications. Now “the adolescent can love freedom and hate exploitation. The possible and the ideal captivate the mind and the feelings”.
Psychosocial development in adolescence
• For Elkin, adolescent thinking contains traits of immaturity reflected in: the tendency of constant discussion in an attempt to affirm their ideas; the insecurity that leads them to indecision, to finally adopt unmeditated and impulsive postures; feeling like they are the center of the world; wishing to be taken into account; the desire to attract attention, believing that they are unique, as if the rules of others did not affect them and, consequently, thinking that no one feels like them.
• For Erikson, the search for identity (understood as the awareness of knowing who one is), is the main task during the adolescent years. Knowing one’s own identity makes the adolescent feel unique and different from all the others. The identity is formed by modeling and imitation, but also by their own modifications that derive from their knowledge, ideas, thought and education. Identity confusion is a risk that can last into adulthood. Adolescents consolidate their sense of personal, sexual and social identity, building a positive or negative theory about themselves, which will have a decisive importance for the rest of their lives, since self-esteem and the feeling of ability to manage their own lives autonomously, responsibly and effectively are based on it.
• Bandura’s theory of social learning. Our brain is programmed to learn and from an early age one of the most powerful methods of learning is modeling or imitation. Throughout their family, school or social life, adolescents tend to imitate what they like, and more so if it is positively reinforced. Industrial and consumer societies exert a great influence on the learning of adolescents. Therefore, the people who most influence adolescents may be public, famous or successful figures.
• Cultural mistreatment (F. López). Socially prolonged adolescence is a cultural creation. Industrial societies produce this social prolongation of adolescence, either because they can afford it, extending compulsory schooling, or because if they are in crisis they cannot offer work to a good part of adolescents. From the social point of view, adolescence should entail a certain degree of autonomy of the young person from his family in numerous aspects of life: the bond of attachment continues to be fundamental, but with less need for proximity and family presence.
Epidemiological situation of adolescence
In 2016, in the world, there were 1,800 million adolescents and young people between the ages of 10-24. There is growing inequality and greater challenges for the health of today’s young people than those that this same group had to face 25 years ago.
Adolescence, from the point of view of public health, is a stage to which attention must be paid, not only in industrialized countries, but in all others. In 2011, the Lancet journal published a study on mortality by age groups of 5 years, from birth to the end of adolescence. The conclusions, among others, were: death rates in 15-year-olds are higher than in those under 10 in high-, middle-, and low-income countries, and most deaths are caused by injuries. These data highlighted the importance of investing in preventive health measures in adolescents throughout the world.
In the world, according to data from 2016, there were 1,800 million adolescents and young adults, between 10-24 years old, which constitutes a third of the world population. There is a growing inequality and greater challenges for the health of today’s young people than those that this same group had to face 25 years ago(3,4).
From 1990 to 2021(5,6), there have been notable changes in adolescent health. A decline in the burden of disease in many countries has been offset by growth in the adolescent population in poorer countries. Overweight, obesity and anemia have increased. Child marriage is prevalent, with an estimated 66 million women between the ages of 22 and 24 being married before the age of 18. Although globally, there is gender parity in secondary school completion, the prevalence of NEETs –youth without education, employment or training– remains higher for young women in multiburden countries, suggesting few opportunities to enter the labor market.
According to WHO data in 2021(6): half of all mental health disorders in adulthood begin before the age of 14, but, in most cases, they go undetected and untreated. Substance abuse affects young people disproportionately compared to older people. The fact of starting substance use early is associated with a higher risk of falling into dependencies and other problems during adult life. Globally, 43 out of every 1,000 girls between the ages of 15 and 19 give birth each year.
The global burden of disease has changed little since 1990 and the prevalence of many adolescent health risks has increased(6,7). Health, education, and legal systems have not kept pace with the changing needs of adolescents and changing demographics. Gender inequity remains a powerful driver of poor adolescent health in many countries.
As of January 2021, according to the Spanish National Institute of Statistics (INE), there were 5,954,862 adolescents in Spain between the ages of 10 and 21 (12.5% of the total population). This number has remained stable in recent years.
Mortality. Progression
The leading causes of death for adolescents are injuries and trauma (including road traffic and drowning), violence, self-injurious behavior, and maternity-related ailments. Most are avoidable.
In the world, according to a recent study by the WHO 2021(6):
• In 2019, more than 1.5 million adolescents and young adults between the ages of 10 and 24 died, which is almost 5,000 a day.
• Of all the age groups, the one with the lowest risk of death is that of young adolescents between 10 and 14 years of age.
• The leading causes of death for adolescents and young adults are: injuries and trauma (including road traffic and drowning), violence, self-harm behaviors and maternity-related ailments.
In most cases, these are avoidable deaths, both those caused by external causes (violence, traffic accidents, etc.), and those related to infections (through vaccinations, improving access to the health system, etc.). Boys die more in the context of violence and girls from situations related to motherhood. Despite these data, it must also be taken into account that the causes of mortality are different depending on the country.
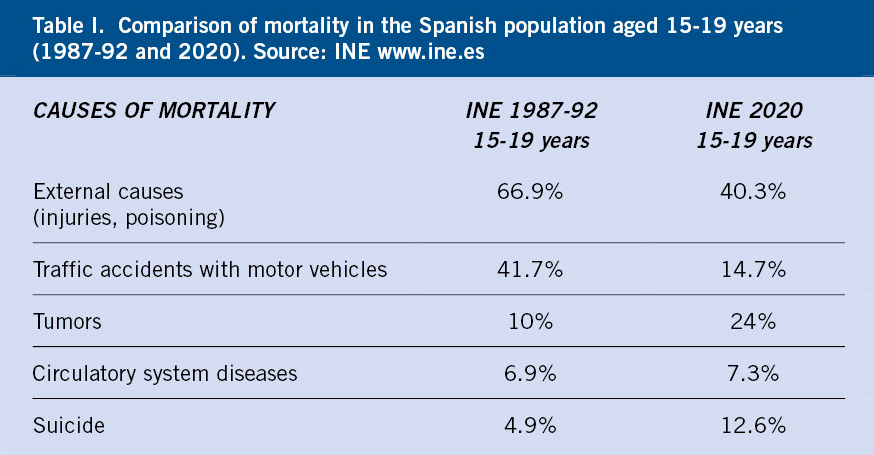
In Spain, according to INE data, in 2020, mortality between 10-19 years of age was 11%(8). The main causes among 15–19-year-olds were: external causes, 40.3% (traffic accidents, violence, suicide and self-inflicted injuries), followed by tumors-neoplasms, diseases of the circulatory, respiratory and nervous systems. In Table I we can see the differences in mortality that occurred in our country between 1987-92 and 2020, with a significant decrease in external causes and, especially, in traffic accidents, which has been maintained in recent years. On the other hand, tumors and suicide are especially relevant, and with a tendency to increase, as a cause of death in this stage. The latter is increasing significantly in these last two years of COVID pandemic.
Morbidity. Reasons for consultation. Causes of hospital admission
All the pathologies and risk factors that are avoided or corrected during this period will serve to have healthier adults in the future.
In general, adolescence is a period of health from the biological point of view, although it is a period of many risks. It is important not to forget that those pathologies or those health risk factors that are avoided or corrected during this period will serve to have healthier adults in the future.
The problems that adolescents present, in general, are a consequence of their psychological and social development (mental problems, risk behaviors), their biological development (scoliosis, acne, dysmenorrhea, trauma problems, etc.), infectious diseases (as in any other time of life, so it is essential to continue vaccination at this age), adult pathologies that can be detected asymptomatically during this stage (hypertension, hyperlipidemia, obesity, diabetes) and chronic diseases, of which in the past, patients died before reaching adolescence, such as: congenital heart disease, cancer or chronic diseases, for example, cystic fibrosis of the pancreas.
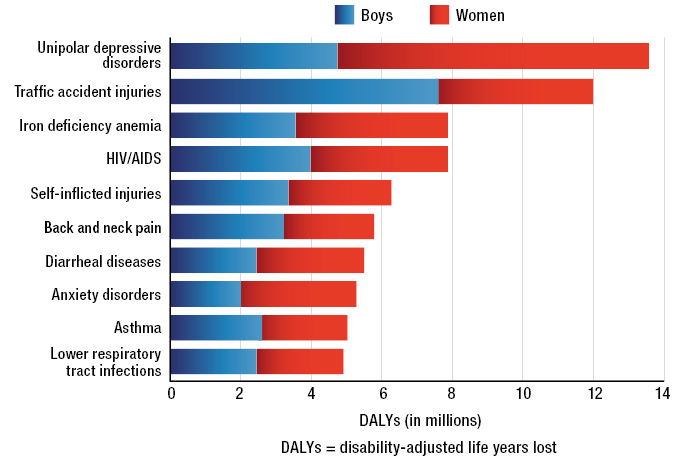
At a global level, according to studies by the WHO 2014(4), the main causes of disease by years of life lost adjusted for disability and by sex, can be seen in Figure 1. Although it is not reflected on the list, it should be noted that malnutrition is on the rise. Undernutrition in low-income countries and obesity increasing in both low- and high-income countries.
Figure 1. Leading causes of disease by years of life lost, adjusted for disability and by sex. Source: WHO Health for the world’s adolescents. A second chance in the second decade. 2014 (online). Accessed February 2022. Available at: https://apps.who.int/iris/ handle/10665/141455.
Morbidity. Some data of Spain(8)
• Drugs. The ESTUDES 2020 Survey (2018 data), has been carried out since 1994, every two years, on the use of drugs in secondary education, from 14- to 18-year-olds(9). The 2020 data confirms that the consumption of alcohol, tobacco and cannabis, which had been declining, has stabilized in recent years. 77.9% had tried alcohol at some time. 41.3%/33% had smoked tobacco/tried cannabis at some point, respectively. Cocaine use decreases, and ecstasy use slightly increases. The consumption of other substances (hypnotics, hallucinogens, amphetamines, volatile inhalants, heroin, etc.) is much smaller, with less than 2% of adolescents who have tried it.
• Problems related to sexuality. According to INE data in 2011, the rate of births per thousand (or fertility rate) between 15–19-year-olds was 11 and has been progressively decreasing, thus in 2017 it stood at 7.15. The voluntary interruption of pregnancy (VIP) in the same age group, in 2011 was 14.09 and has continued to decrease to 7.41 in 2020, although it is not known for sure, since spontaneous abortions cannot be counted.
If we add the number of births in individuals younger than 19 years of age plus VIPs (although this figure is not exact) in the same age group and during 2019, we obtain 17,500 pregnancies in those under 20 years of age/year, a very important figure to take into account.
The average age of the first complete sexual relationship, according to data from INJUVE 2020, is 16.2 years. 50.2% of adolescents aged 16-18 have had complete sexual intercourse (Observatorio S.E. Contracepción 2019).
62.5% of adolescents (87.5% men, 38.9 women) between 13-17 years of age have seen pornography at some point in their lives. The beginning is around 12 years of age and almost 50% have put it into practice. The danger is that their sexual desire is being built on unreal, violent and uneven foundations typical of fiction (Save the Children 2020).
Regarding sexually transmitted infections (STIs) in adolescents, we know that they are sometimes asymptomatic and can cause serious sequelae, such as pelvic inflammatory disease, infertility or cancer. Adolescents, in general, take time to consult, even if they have symptoms, a third of them do not perform the treatment adequately, which entails a greater risk of sequelae; there is insufficient use of condoms and, currently, HPV vaccination in the Interterritorial Calendar of our country is still not recommended for men, and vaccination coverage is insufficient in women.
• With regards to nutritional problems, such as obesity, although it is difficult to compare the studies due to the different methodologies, in the Paidós-84 study, the prevalence (6-13 years) was 4.7. In the Enkid-2003 study (2-24 years), it was found that 13.9% were obese and 26.3% overweight. In those 20 years, the prevalence of obesity tripled. Santa Cruz in 2012 (8-17 years), obtained a prevalence of obesity of 12.6 and overweight of 26%. In these last two years of the COVID pandemic, the prevalence of obesity has increased due to sedentary lifestyle and altered nutritional habits.
Also, the prevalence of eating behavior disorders (ED) in adolescents has increased. 70% of adolescents are not comfortable with their body; 6 out of 10 girls would be happier if they were thinner and 30% reveal pathological behaviors.
• Mental health. 20% of Spanish adolescents (10-19 years old) suffer from a mental health problem, more so in women (UNICEF-Mental state of childhood 2021).
• Technologies. Its use is very high (computer 91.5%; Internet 94.5%, mobile 69.5%), being higher in females. The relationship between the use of social networks and dysfunctional behaviors on the Internet is well established.
• Bullying affects 10-15% of students.
• Early school/training dropout between 18-24 years of age is 20.2% in men and 11.6% in women (Europe 2020 Ministry of Education and FP).
Despite these data, adolescents feel healthy and do not have the perception that their behaviors are risky, so they do not usually go to health services, unless they need it due to significant acute pathology. Sometimes they are unaware of who their doctor is or they do not trust him. On the other hand, health professionals, in general, have shown little interest in this age group.
Any consultation with a young person must be used to the maximum and, although the concern that has brought him or her is attended, prevention must be carried out. Whenever you are dealing with an adolescent, the “hidden agenda” will be taken into account, that is, that they may attend the clinic for a problem and what really worries them is another; for example: a young woman may consult for abdominal pain and what worries her is a possible pregnancy or STI. She may go for dizziness or headache and what underlies is that she has problems at school, at home or with her partner.
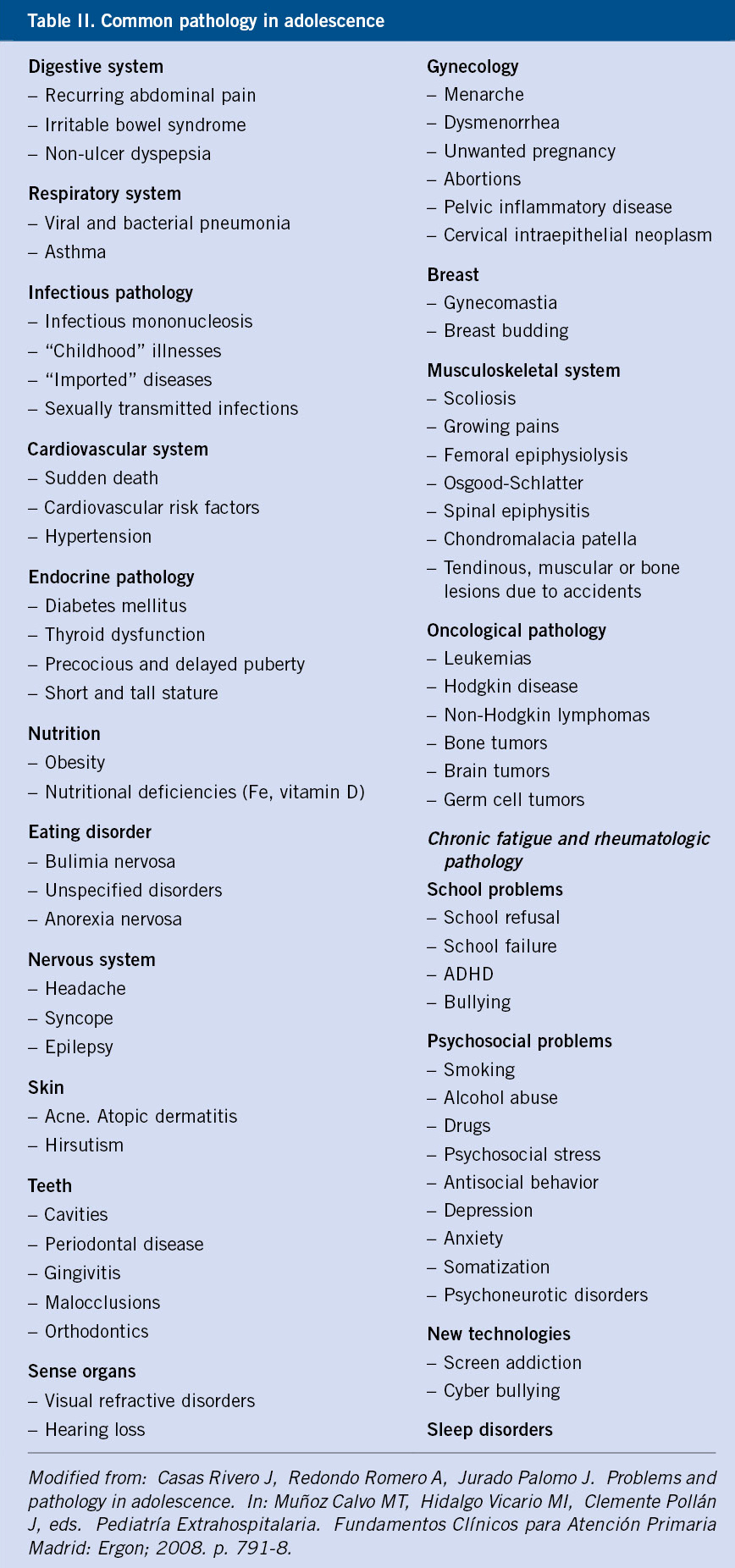
Reasons for consultation
The acute pathology is what makes the young person attend the consultation (Table II) and, in general, these problems are scarce, both for Primary Care, hospital Emergency Room or Specialist consultations. There are a few studies looking into this since its investigation is complex, due to the hidden agenda of the young person, the high rate of psychosomatic pathology –which makes diagnosis difficult–, and the differences according to the place where one consults –general clinic or young persons’ clinic(10)–. In the latter case, most consultations are related to sexuality and unwanted pregnancy.
In a study carried out looking into the reasons for consultation between 10–18-year-olds in a General Consultation Health Center(11), the following were obtained from higher to lower frequency order: ENT infections (45.3%), skin problems (24 %), trauma (15.3%), allergies (7.6%) and gastroenteritis (7.6%). Consultation for issues related to sexuality, drugs or personal problems were very low: less than 3%.
Reasons for hospital admission
According to the study by Díaz Gañán (2009)(12), the most frequent causes of hospital admission in the Community of Madrid, in male adolescents aged 15-24 years, from highest to lowest frequency were: injuries and poisonings 18.1 %, gastrointestinal problems 17.2%, musculoskeletal and connective tissue issues 15.1%, and respiratory disorders 11.6%. The causes in women were: complications of pregnancy, childbirth and puerperium 50.6%, digestive system 10.2%, respiratory system 5.5% and injuries and poisoning 3.5%.
Romero et al., in 2006, found that the most prevalent reasons for admission to an Adolescent Medicine unit between 13-16 years of age were the management of chronic diseases in both sexes; followed by: traumas, confusional state/syncopes and intoxications. The patients who were admitted for organic conditions associated undiagnosed underlying psychosomatic conditions.
We still do not possess a tool that accurately measures the health needs of adolescents. There is a biomedical pathology that appears in all the databases and that reflects reality well; but there are other pathologies, such as psychosomatic ones, those related to body image, lifestyle or affective deficiencies, even with the so-called secret pathologies related to personal situations experienced with intensity and that alter emotional stability, which are not reflected in the studies.
Pathologies prevalent during adolescence
Adolescents suffer from different pathologies and many are related to their risk behaviors. Due to medical advances, there has been a change in relation to chronic diseases, in which infant mortality has reduced and life expectancy increased, even into adulthood. Strategies are needed to achieve greater involvement and adherence to treatments.
Subsequently, the most frequent pathologies that can be found during adolescence are briefly presented(10,13,14).
• Accidents. They constitute the main cause of death and disability in the group between 15-24 years of life, with a significant proportion being traffic accidents. It has been estimated that the correct use of the seat belt while driving could reduce the risk of injury by 45-55%, and mortality by 40-50%, both for the driver and the passenger. In addition, advice should be given against alcoholic beverage consumption if need to drive, since alcohol is related to traffic accidents in 40%. The use of a helmet when cycling reduces the incidence of head trauma by 69-80% and its use on a bicycle or motorcycle reduces the risk of injury or death (Evidence II-2; Recommendation B).
• Drugs. Its use is associated with: traffic accidents, homicides and suicides, early sexual activity, school failure, mental disorders, family problems and delinquency; in addition to the possible consequences in adulthood, such as: cardiovascular diseases, psychiatric disorders and cancers. Legal drugs (alcohol and tobacco) are the most prevalently used and are the gateway to other drugs. In high-income countries, the pattern of consumption characteristic of young people is maintained: multiple consumption, in recreational environments, during the weekend; the percentage increases with age and female consumption is rising.
• Problems related to sexuality. The increase of unwanted pregnancies and STIs in adolescents is a consequence of: early menarche, early onset of sexual relations, inappropriate use of contraceptive methods, existence of multiple partners, drug use and ignorance. Young people, due to: their physiology, their late consultation, lack of correct treatment compliance, etc., have a higher risk than adults of morbidity and long-term sequelae, such as: infertility, pelvic inflammatory disease, ectopic pregnancy or cancer. It is important to encourage HPV vaccination, both in women and men, as it prevents cancer.
• Nutritional disorders. Excessive calorie intake is a more serious and important problem than inadequate intake. In various studies in Western countries, a high consumption of saturated fats and low carbohydrates has been observed, as well as an insufficient intake of dairy products and fruits, with the consumption of fast food being increasingly widespread, which leads to an excess of saturated fats, sodium and refined sugars, with a high caloric intake, and almost no intake of vitamins and minerals, accompanied by an increase in the prevalence of overweight and obesity. In Spain, the figures for the prevalence of childhood and adolescent obesity, as previously mentioned, have tripled in the last 30 years. Eating disorders are increasingly occurring at younger ages, and encompass a wide spectrum, from subclinical and partial symptoms, even severe clinical pictures with serious consequences if they are not treated. They have irreversible complications: growth stagnation, failure to achieve the peak bone mass, and brain changes. Bigorexia, is more frequent in males who are obsessed with the practice of sports to obtain an athletic body and they prioritize it before any other activity. Orthorexia is the obsession with eating healthy food, knowing its origins and process until it reaches the consumer. In relation to all this, there is also a great demand for aesthetic interventions to improve appearance (breasts, nose or abdomen), as well as the significant increase in the consumption of clothing, fashion, computers…
• Mental health. Emotional and behavioral disorders. The conflictive situations typical of adolescence, together with the fragility of their developing personality, constitute an ideal framework for the emergence of possible mental disorders. Girls are more likely to have emotional problems (anxiety, depression) and eating disorders; boys are more vulnerable to disruptive and violent disorders. In the last two years of the COVID pandemic, mental problems have multiplied significantly.
• Information and Communication Technologies (ICTs). ICTs have revolutionized today’s world, they are present in most homes/schools and they constitute a danger for adolescents. Children begin their use when they have not yet developed the ability to understand terms, such as respect for oneself and others, privacy or intellectual property. The information that is posted will last forever (fingerprint). Its use entails many educational, communicative or entertainment benefits, but also many risks that must be taken into account: violence, pornography, addiction, identity theft, school failure, emotional, psychiatric disorders, visual disturbances (myopia, fatigue, dry eyes from decreased blinking), headaches, in addition to cyberbullying, grooming and sexting. Popularity today is measured by the number of followers on social networks. We are the first generation in history in which, on a massive scale, technology transfer is carried out from children to parents, and not the other way around. Adults, in general, are unaware of the technical aspects and underestimate the possible risks, although in recent years this has been changing.
• Sleep disorders. Different studies have shown that children and adolescents sleep an insufficient number of hours for their needs, which can affect: their physical and mental health (impaired growth, obesity, hypertension, immune disorders, emotional and behavioral problems); their safety (accidents); academic success and quality of life, conditioning chronic sleep disturbances in the future. According to different studies, up to 30% of children and adolescents will present some disorder and/or sleep problem. This is influenced by the biological changes of puberty and causes that are modifiable, such as: lifestyle and habits, use of technologies, academic demands or early start of classes. The most frequent disorders during adolescence are: insomnia, parasomnias, restless legs syndrome and delayed phase syndrome.
• Chronic illness or disability. As mentioned, the adolescent population is, in general, a healthy population. However, mainly due to medical advances, a change has been seen in relation to chronic diseases, in which infant mortality has been reduced, and life expectancy increased, even into adulthood. These medical achievements represent an increase in adolescents with chronic diseases: asthma, neoplasms, heart disease and other congenital malformations, diabetes, epilepsy, inflammatory bowel disease, myopathies or metabolic disorders, among others.
If a chronic disease causes difficulties at any time in life, during adolescence, some special elements are added. For example, on the one hand, he is a patient who is in a vital phase in need of an autonomy that we must promote, but who, in turn, on some occasions may not accept or understand the implications that the disease has, and may also not be involved in self-care (taking medication, attending medical appointments…). Sometimes, if the adolescent does not get involved, it may happen that the parents/guardians become too involved, or that they disengage, generating conflicts, bad progress of the disease, increase in the number of hospital admissions, etc. But precisely because of the increase in life expectancy of these diseases, which suggests that adolescents will reach adulthood, it is of great importance that strategies are found to achieve greater involvement and adherence to treatment.
Adolescents with chronic illnesses are as likely or more likely than their healthy peers to engage in risky behaviors. Also, they are more prone to have emotional disorders and depression, being victims of different forms of violence, bullying, maltreatment and sexual abuse. Likewise, they present a poor adaptation to the health system and, on occasions, denial of the disease, in addition to severe side effects due to the medication they take. Although care during the transition process is important for all adolescents, it is more relevant in this case.
The transition process
Transition is understood as: the process of preparation, adaptation and gradual integration of children and adolescents in an adult care unit.
Life is a continuum. It has been the health managers and the complexity and sophistication of the treatments that have forced the division of medical care.
Each stage of life has certain characteristics and needs a type of assistance. In fact, each field requires a different professional profile and this is sometimes not well understood by patients. The characteristics of each stage of life make us put on the table how the passage from one stage to another in health care occurs, that is, the patient’s transition from one specialty to another. With regards to adolescents, it must be added that young people change quickly and significantly, which requires adaptation, both on their part and on that of the professionals who care for them, if the aim is to achieve the maximum care quality, efficiency and clinical success(15). The two main objectives of a well-organized and coordinated transition are to optimize health and make it easier for the adolescent to feel satisfied with health care(15).
We can distinguish two types of assistance: Primary Care (PC) and Specialized Care (SC). The first is given in Health Care Centers and, although it deals with comprehensive health care, it also cares for healthy adolescents, it is based on: Health Education (HE), Health Promotion (HP) and Primary Prevention (PP). The second, takes place in hospitals and mainly cares for patients with chronic pathology, almost always multidisciplinary. In both cases, the care transition has specific characteristics.
The transition in Primary Care
In most of the Spanish Autonomous Communities, the age limit for healthcare is 14 years old and, in some, it reaches 16 years old. Although certain professionals continue to care for adolescents beyond this age, in the health check-up clinic between 14-16 years of age, the patient’s parents are usually informed that from that moment the administration transfers their data to the family doctor’s office. This step should be taken more seriously by everyone: pediatricians, family doctors, nurses, family and coordinated actions should be carried out.
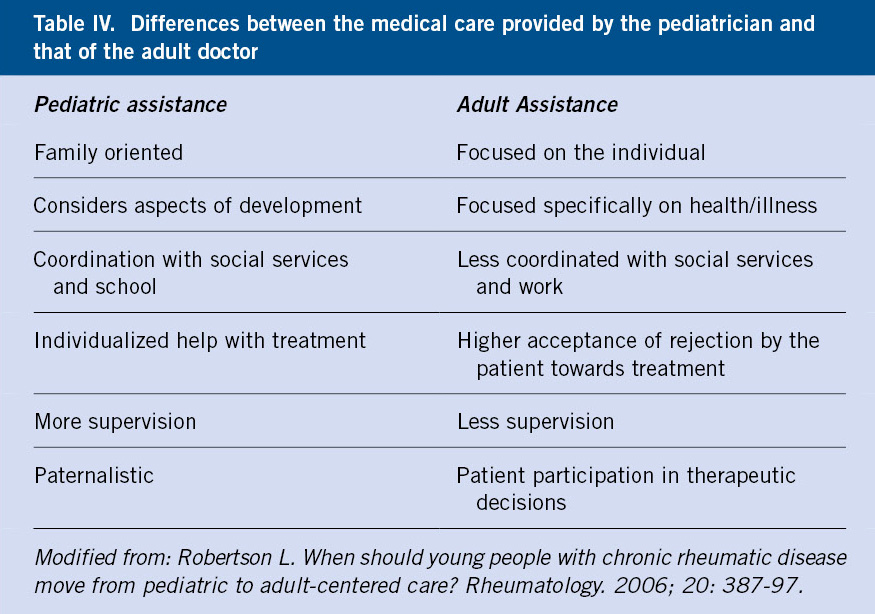
If we start from the conceptual basis that adolescence is a stage that unites childhood with the adult state, the coherent action would be to maintain attendance, at least, during the minimum time that the stage lasts, up to 18 years of age. But reality differs, rather assistance is interrupted in middle adolescence (14-16 years), the most critical moment of the entire process. It is poorly understood how a 14-year-old child, when his/her growth and development has not yet concluded, should transfer from individualized, supervised, family-oriented Pediatric care coordinated with the school and the environment, to an adult-oriented care, much more impersonal, focusing on the health-disease axis and not on aspects of development. The change from pediatric care to the adult model entails an important break, and sometimes leads to loss of follow-up and adherence to treatment and also increases the number of patient admissions(16,17).
The transition, as we suggest it, could be considered a “rite of passage-initiation”, which recognizes the age of the adolescents who are given autonomy to use health services according to their criteria and needs. The transition is the time to recapitulate the entire stage that has taken place since birth and talk about health as an important value in life. It is about contributing to promote the “principle of patient autonomy”: “the patient’s right to decide for himself about the acts that will be performed on his own body and that will directly or indirectly affect his health, his integrity and his life”.
The transition is specific to each person and should occur between the ages of 16-18 (depending on how care is organized) and, more important than age, the transition should take place when young people are mature enough to do so and have sufficient skills for self-care(17). Not all adolescents have the same degree of maturity and autonomy to manage the control of their health. The law gives the right to decide about this from the age of 16 (legal health age), when it is considered that their decisions do not seriously risk their health. The level of development is also not the same in all adolescents. There is a TRAQ questionnaire (Transition Reading Assessment Questionnaire) that aims to measure this autonomy through an assessment. It is an instrument that assesses the abilities of adolescents with chronic diseases in relation to autonomy and self-care that they acquire in the transition to adulthood. It is aimed at people between 14 and 26 years old and the questions are classified into 5 domains: use of medication, attendance at appointments, follow-up of health problems, communication with professionals and management of daily activities(18).
Transition is a dynamic process, not an event, it must be gradual and multidisciplinary, since it implies a process planned over time to prepare for medical, psychosocial and educational needs in adult services. Coordination between services is essential. There are three stages: initial, when the decision is made; intermediate, the patient, his family and his doctor are already prepared; and finally, when the adolescent or young adult, in addition to being “transferred” to an adult service, actively participates in their care and decision-making, according to their abilities. There are obstacles to the transition, dependent on the patient, family, pediatrician or adult physician(17). During transition, there is the presentation of other professionals who will be involved in their health care. On one side, not all professionals have the same way of understanding clinical practice; on the other hand, adolescents are very sensitive to forms of treatment and, if these are not appropriate, they can ruin the clinical relationship.
In a study carried out in 2021 in Spain, it was found that 75% of young people had visited the family doctor before turning 21, while the remaining 25% finished this stage without making any appointments. It is noteworthy that they attended the consultation for the first time at a very young age, in most cases at 15 years old (67%) or 16 years old (20%). It can be interpreted that this early initial visit is due to the adherence of patients to the Pediatric consultation, which is transferred to the first visit with their adult doctor(18-19).
Adolescent morbidity and mortality, as previously mentioned, is highly relevant. At this age, Health Education (HE), Health Promotion (HP) and Primary Prevention (PP) are very important. That is why the term “opportunistic recruitment” is used, that is, taking advantage of each medical act to implement preventive programs. In addition, it could be attempted that, from the age of 16, the patient attended the consultation by himself, thus eliminating biases in the collection of information and promoting the autonomy, independence and capacity of the young person, facilitating accessibility to the system as an adult patient whom we are going to accompany as long as we can and is need(20).
In the last six years, programs have been established in our country to carry out the transition at the hospital level, and its organization in Primary Care (PC) is also required. It is necessary, when the time comes, to establish visits to the adolescent’s Health Center with the two professionals (the pediatrician to introduce the adolescent and explain his or her health problems and needs, and the family doctor who receives the adolescent) to carry out the transfer.
The transition in Specialized Care. Patients with chronic diseases and disabilities
WHO considers chronic diseases as: “those diseases that have a long duration (more than 6 months) and a slow progression, are not transmitted from person to person and are considered, therefore, non-communicable”. The use of the term “adolescent in need of special health care” has been proposed as a less stigmatizing and more socially acceptable term (Stein. USA). In recent decades, we have witnessed an increase in the prevalence of chronic diseases ranging between 10 and 30%(20). Globally, 9 out of 10 children affected by a chronic disease will exceed 20 years of age(15).
We understand by transition: the process of preparation, adaptation and gradual integration of children and adolescents with a chronic pathology in an adult care unit. The transition process begins in early adolescence but does not end until the young adult is fully integrated into an adult unit. However, the term transfer refers to the moment of transferring the patient with clinical and administrative information from one pediatric unit to another unit for adults (it does not imply development, it is not a process but a moment)(18-19).
Many adolescents are transferred abruptly, either because they have reached a certain age, or because of an acute decompensation that motivates admission to an adult service. Preparation for this step and coordination of care between the pediatric and adult groups are essential to facilitate the transition process, which must ensure the same quality and continuity of care for these patients, especially in the case of chronic diseases(16).
The American Academy of Pediatrics (AAP), the American Academy of Family Physicians (AAFP) and the American College of Physicians (ACP) have been aware of the importance of the medical care process in the adolescent’s transition from the pediatrician to the family physician, and the need to give more autonomy in their health care, especially to those who suffer from a chronic disease. The aforementioned organizations drafted a manifesto called: “The six main elements of the transition”(21), which are:
1. Beginning of transition: to talk with the patient and family about the plan and conduct training of the implicated staff.
2. Care and monitoring of the transition process, tools to establish criteria for inclusion, selection, observation, registration, etc.
3. Patient training: aims to assess their abilities and prepare them for a correct transition.
4. Transition planning with individualized preparation of the patient: objectives, detailed report, information to the family doctor and choosing the best moment for the transition, counseling for patients with intellectual disabilities, as well as help in choosing the adult doctor and coordinating with him.
5. Medical transition with all the clinical history and additional information to the adult doctor, when the disease is in a stable phase. It is the responsibility of the pediatrician to care for the adolescent until he is seen in the adult consultation.
6. End of transition. The pediatrician is to contact with the family and the patient so as to end the relationship, and offer the necessary help and contact with the adult doctor, as well as build collaboration alliances with the rest of the professionals.
In short, transition plans need to be elaborated together with the patient and family, starting the process at 14 years of age and the staff must be trained in the procedures for the correct transition (see Algorithm).
Clinical assistance to adolescents
Currently, there is a care gap with adolescents. In spite of all the aforementioned problems that these present, the doctors show little interest in the health of adolescents. Sometimes their rebellion, arguments, vindication, jargon, exacerbated criticism, disrespect, etc., make them unpleasant and their attention and care unrewarding. That is why it is said that it is the most abandoned stage of life, even more so than old age. There are few plans and programs in the social services portfolio that deal with these stages in detail. We have a history that can justify it. Until well into the 1990s, the age limit for pediatric care was 7 years. From 1973 to 1982, there is no single publication in Anales Españoles de Pediatría on adolescence. Professionals, rather than institutions, have been the first to give warning of this situation, and all this hand in hand with important social problems, such as: the prevention of substance use, school problems, family conflicts, unwanted pregnancies(1), etc.
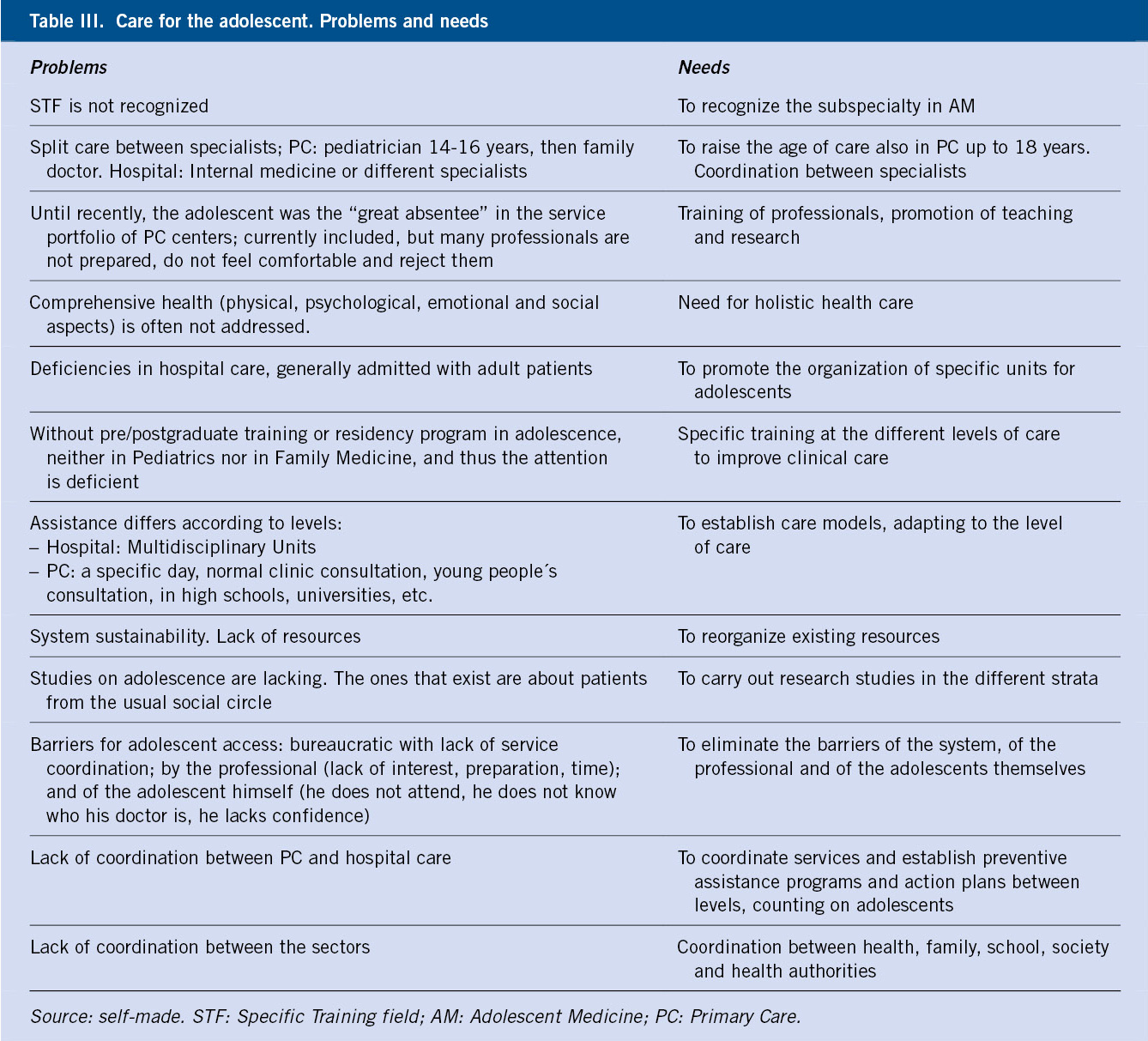
In recent years, several advances have been made, such as the extension of the age of pediatric care to 14-16 in Primary Care (depending on the different Autonomous Communities) and up to 18 years at the hospital level (II National Strategic Plan for Childhood and Adolescence 2013-2016), although without developing a specific strategic plan for its implementation, which includes specific training for health professionals or an increase in resources. However, care for this population is not adequately organized, there is a lack of adequate services, well-trained professionals, as well as recognition of this subspecialty, among others(22). Table III shows the problems for the care of the adolescent population, as well as the needs to solve it.
Various organizations, such as UNICEF in 2011, recommend investing in adolescents: because they need to develop their skills and abilities to become competent, exercise their rights and access quality education and health services, decent employment and participate in a positive way in the life and future of the country.
Global strategic plans
WHO, UN and various organizations are interested in studying the health indicators of adolescents and have created special organizations for it.
The demographic data mentioned above have led WHO and UN to create agencies in charge of studying criteria to measure the health of adolescents.
• Global Strategy for adolescent health 2016-2030(3):
– The Strategy, which is closely aligned with the Sustainable Development Goals (SDGs), seeks to ensure that adolescents can exercise their rights to health, physical and mental well-being.
– It aims to put an end to the preventable mortality of adolescents in any environment and part of the world by 2030 and guarantee universal access to health services. To this end, the Global Strategy provides a work plan that aims to set the milestones to be achieved by the different countries between now and the year 2030, taking into account the available evidence of the evaluation of needs and results of the effectiveness of the interventions.
– In relation to adolescents living in contexts of humanitarian crisis, the Global Strategy warns that they present a higher risk of morbidity than the general population, due to the conditions of insecurity, sexual violence and depression to which they are exposed. It urges the global community to act more quickly and invest more resources in helping people at risk.
– It integrates health in all policies, in particular with regards to: malnutrition, air pollution, poor water quality, sanitation and hygiene, violence and harmful and discriminatory practices.
– It defends the adoption of equity-oriented policies and programs that are based on human rights, especially for adolescents in situations of social exclusion and marginalization.
• Measuring adolescent health: a necessary step towards achieving the global goals. In 2018, the Global Action Advisory Group for Adolescent Health Measurement (GAMA) proposed a project sponsored by WHO and the support of other agencies, such as United Nations (UN) and the Bill and Melinda Gates Foundation, to search for indicators of adolescent health, knowing that one third of the global burden of disease is attributable to the behavior and circumstances of adolescence(23-25).
– GAMA accepts the age group that WHO considers adolescence between 10 and 19 years, but admits other definitions. Both health problems and social or health care systems change in these years. They recognize that young adults feel better served in older adolescent settings. Work is carried out in collaboration with local governments interested in improving the lives of adolescents.
– GAMA plans to stimulate the use of health indicators. The impact of these recommendations at national level will depend on the support within each country.
– UN Sustainable Development Goals (SDGs) require all countries to: pay attention to equity, prevent poverty, promote health and general economic growth, address education, social protection, employment, climate change and environmental protection.
– Investing in services for adolescents is a priority and this requires a political commitment from all nations to improve the lives of young people.
– The Alliance for Maternal and Child Health and many other WHO-recognized organizations are committed to improving adolescent health. They made a calling for the well-being of adolescents in 2019, which was to engage and empower adolescents and strengthen political commitment for funding through the World Summit on Adolescents in 2023.
– The importance of youth participation in the SDGs, UN and WHO increases the effectiveness of plans and strategies. The Secretary General of UN highlights the importance of the fact that 1,800 million people between the ages of 10 and 24, who have become agents of change, have enormous potential to achieve a better world.
Role of the Primary Care pediatrician
The work of the pediatrician extends beyond the treatment of the disease or its complications, and must care for and accompany during this period, so that the patient reaches adulthood with: the best quality of life, the least number of complications and without suffering during the transition from the pediatric model to the adult model (Table IV). The pediatrician needs to know the characteristics of adolescents, their needs and health problems, as well as their family and social dynamics.
As we know, the adolescent seldom attends the clinic, the pediatrician must make the most of his visits to address all the issues that influence his overall health, and also carry out education and prevention. For this, the acronym proposed by the Spanish Society of Adolescent Medicine (SEMA) can help: F.A.V.O.R.E.C.E.R. (=PROMOTE health): Family, Friends, Healthy life-vaccinations, Objectives-leisure, Religion-spirituality, Self-esteem, School-university-work, Mental state, Risks).
Conflict of interest
There is no conflict of interest in the preparation of the manuscript. Declaration of interests: none.
Bibliography
Asterisks show the interest of the article in the opinion of the authors.
1.** Rodríguez Molinero L. Biopsychosocial health of adolescents in Valladolid. Doctoral Thesis, University of Valladolid. 1993 (in Spanish).
2. Rodríguez Molinero L. The adolescent, the school, the university and their peers. In: Hidalgo Vicario MI, Rodríguez Molinero L and Muñoz Calvo MT. Adolescent Medicine. Comprehensive care. 3rd ed. Madrid: Ergon; 2021. p. 77-83 (in Spanish).
3.** United Nations. Global strategy for women, children and adolescent health 2016-2030 (online). NY. Accessed February 2022. Available at: https://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_16-sp.pdf.
4.*** WHO. Health for the world’s adolescents. A second chance in the second decade. 2014 (online). Accessed February 2022. Available at: https://apps.who.int/iris/handle/10665/141455.
5.** Azzopardi PS, Francis KL, Hearps SJC, Mbiostat KLF, Kennedy EC, Mokdad AH, et al. Progress in adolescent health and wellbeing: tracking 12 headline indicators for 195 countries and territories, 1990-2016. Lancet. 2019; 393: 1101-18.
6.*** Adolescent and young adult health. WHO. January 2021 (online). Accessed February 2022. Available at: https://www.who.int/es/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions.
7. Inter-institutional Group for the Estimation of Mortality in Children of the United Nations. Levels and trends in child malnutrition: Report 2020 (online). Accessed February 2022. Available at: https://www.who.int/es/news/item/19-09-2019-more-women-and-children-survive-today-than-ever-before-un-report.
8. INE. Statistics National Institute. 2021 population census. National results. General characteristics of the population (online). Accessed February 2022. Available at: www.ine.es (in Spanish).
9. Study STUDIES. Survey on drug use in secondary education in Spain, 1994-2021. Ministry of Health. Government of Spain. 2021 (in Spanish).
10.** Salmeron Ruiz M, Casas Rivero J, GuerreroAlzola. Health problems in adolescence. Chronic pathology and transition. Pediatr Integral. 2017; XXI: 245-53 (in Spanish).
11. Menendez Suso JJ, Hidalgo Vicario MI, González Rodríguez MP, Parra Martínez MI, et al. Reasons for consultation of adolescents in a Primary Care center. Communication presented at the XV National Congress of the Spanish Society of Adolescent Medicine. Grenade; 2003 (in Spanish).
12. Díez-Gañán L. Hospital morbidity, Community of Madrid, 2008. Epidemiological bulletin of the Community of Madrid nº10. 2009; 15: 26-7 (in Spanish).
13.** Vallejo Matavera V, Rodríguez Molinero L, Hidalgo Vicario MI. Current situation of adolescence. Epidemiological data: morbidity, reasons for consultation and mortality. In Hidalgo Vicario MI, Rodríguez Molinero L and Muñoz Calvo MT, eds Medicina de la Adolescencia. Atención Integral. 3ª ed. Madrid: Ergon; 2021. p.1-9 (in Spanish).
14.** Hidalgo Vicar MI. Comprehensive adolescent care. critical review. XVIII National Congress of the Spanish Society of Pediatrics Outpatient and Primary Care. Comprehensive Pediatrics. 2004; 7: 76-84 (in Spanish).
15. Raiola G, Galati MC, Socavones M, Talarico V, Chiarello VP. The transition of care from the adolescent to the family doctor. Adolescere. 2017; V: 14-21 (in Spanish).
16.** Suris Bulk JC,Barrense-Dias Y, Akre C. The adolescent with chronic illness and disability. The transition. In: Hidalgo Vicario MI, Rodríguez Molinero L and Muñoz Calvo MT. Medicina de la Adolescencia. Atención Integral. 3rd ed. Madrid: Ergon; 2021. p. 1325-8 (in Spanish).
17. Hidalgo Vicar MI. The transition of the patient with chronic diseases. Comprehensive Pediatrics. Pediatr Integral. Editorial. 2013. XVII; 157-59. (in Spanish).
18. Ayechu Díaz A. Transition from adolescent care to family doctor. Adolescent autonomy. Adolescere. 2021; IX: 75-80 (in Spanish).
19. Otero Arévalo E. The transition from the adolescent to the family doctor. Analysis and improvement proposal. Adolescere. 2021; IX: 81-8 (in Spanish).
20. Barrio Cortes J, Suarez Fernandez C, Bandeira de Oliveira M, Muñoz Lagos C, Beca Martínez MT, Lozano Hernández C, et al. Chronic diseases in the pediatric population: comorbidities and use of Primary Care services. Anales de Pediatría. 2020. 93: 183-93.
21.*** American Academy of Pediatrics, American Academy of Family Physicians and American College of Physicians, Transitions Clinical Report Authoring Group. Clinical report- Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011; 128: 182-200.
22.** Hidalgo Vicar MI. Adolescence. Healthcare perspectives. Adolescere. 2014; II: 130-6 (in Spanish).
23. Guthold R, Moller AB, Azzopardi P, Ba MG, Fagan L, Baltag V, et al. The Global Action for Measurement of Adolescent Health (GAMA) initiative Rethinking adolescent metrics. J Adolescent Health. 2019; 64: 697e9.
24. Klein JD.Editorial. Adolescent health measurement. A necessary step toward achieving global goals. Journal of Adolescent Health. 2021; 68: 836-9.
25. Gago A, Iglesias JL. Chronic disease and transition of care from pediatrician to adult physician. In: Hidalgo Vicario MI, Rodríguez Hernández PJ (ed). I Child and adolescent psychiatry course for pediatricians 1st ed. Barcelona: May Editions; 2019. p. 367-79 (in Spanish).
Recommended bibliography
– Adolescent and young adult health. WHO. January 2021 (online). Accessed February 2022. Available at: https://www.who.int/es/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions.
Global adolescent health problems are presented and solutions offered.
– American Academy of Pediatrics, American Academy of Family Physicians and American College of Physicians, Transitions Clinical Report Authoring Group. Clinical report- Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011; 128: 182-200.
A 6-phase protocol to plan and organize a Transition Program is described in detail.
| Clinical case |
|
George is 15 years old. He has Type 1 Diabetes Mellitus since the age of 13. He presented with tiredness and weight loss. He is currently on insulin therapy and acceptably well controlled. He studies 8th grade in a semi-private school. His father is an industrial engineer and his mother is a housewife. He has another sister who is 10 years old. There is an optimal family structure. His mother attends the clinic because the last weekend at a party he got drunk and returned home assisted by his friends. She tells us that since he started the school year, 3 months ago, he does not feel well, does not perform like the previous year, does not follow a correct diet… A few months ago, he went to the family doctor, who, according to his mother, hardly knows him, and who has sticked to prescribing insulin and test strips for blood glucose control. She goes to the pediatrician’s office, since at the last clinic check-up, at age of 14, he told her that if she ever had any health problems, she could count on him. The case is a model of a bad transition. Jorge is a carrier of a chronic disease (diabetes) and will be dependent on health services for life. The correct procedure would have been to have carried out some form of clinical management with his family doctor and nurse, to meet them, even introduce the adolescent to them so as to familiarize himself with their services (not only dispensing syringes and insulin); so that this last episode would have allowed the adolescent to go to him as administrative manager of his diabetes. |
 Adolescence. Epidemiological situation. Most frequent pathology. Transition
Adolescence. Epidemiological situation. Most frequent pathology. Transition