|
| Topics on Continuous Training |
M.A. Zafra Anta*, C. Merchán Morales**
*Paediatrician. Paediatric Pulmonology Department. Assistant Doctor at University Hospital Fuenlabrada. Madrid. Professor-Honorary Collaborator at the Rey Juan Carlos University. Madrid.
** Resident of Paediatrics. University Hospital Fuenlabrada. Madrid
| Abstract
Cough is a common medical consultation in paediatrics. A distinction must be made between recurrent acute cough episodes due to repeated respiratory infections and prolonged or chronic cough. An assessment should be made if coughing persists beyond 4 weeks. History taking must include particularities depending on age, mode of presentation, the epidemiological situation as well as if the cough is dry or productive and association of symptoms. A decision algorithm is suggested for its management. When dealing with chronic cough, different aetiologies must be taken into consideration depending on age. For patients aged 14 years and younger, paediatric protocols will be followed. For adolescents aged 15 years or more, many authors suggest adhering to adult protocols. Training is advisable in order to recognise the sometimes termed “specific cough points”. Early diagnosis of underlying lung disorders (asthma, bronchiectasis, foreign body aspiration, persistent bacterial bronchitis and others) improves clinical outcomes. |
Key words: Chronic cough; Pediatrics; Antitussive agents.
Palabras clave: Tos crónica; Pediatría; Antitusígenos.
Pediatr Integral 2021; XXV (1): 5 EN – 12 EN
Persistent cough
Prolonged and persistent or chronic cough (lasting more than 4 weeks) is a common reason for consultation; although this has varied during the SARS-COV-2 pandemic. Sometimes it is not sufficiently well studied by clinicians. Parents’ expectations should be taken into account, along with possible contact with smokers, and the most likely causes by age and area of care (rural, urban, region).
Cough is a very common reason for consultation in the Paediatric Department, especially in uncomplicated and self-limited acute viral infections. Prolonged and persistent or chronic cough is also a common reason for consultation. The estimated prevalence(1,2) is 5-7% in preschool age, and 12-15% in older children. Sometimes, however, it is not sufficiently well studied by clinicians. In this regard, acute slowly resolving cough and acute recurrent cough should be differentiated.
In recent years, a great deal of research has been carried out into the causes of chronic cough in adults and children(3). In children, for example, the most common in terms of incidence are post-infectious cough, persistent bacterial bronchitis, bronchiectasis, airway malacia and asthma. In contrast, causes typically encountered in adults, such as gastro-oesophageal reflux, asthma and upper airway syndrome, are predominant in adolescents. This difference is related to the inherent characteristics of children compared to adults regarding the respiratory tract, immune system, and nervous system(4).
In older children, particularly during adolescence, there appears to be a greater susceptibility for the development of psychosomatic symptoms, and the personal impact of chronic symptoms should not be ignored if they affect the social sphere(5,6).
A duration of more than 3-4 weeks is the threshold for distinguishing between acute and prolonged or chronic cough in most paediatric guidelines, and that is the period of time over which it should be evaluated and followed-up. In adults, this threshold is from 8 weeks onwards(7,8).
Only the British Thoracic Society considers cough in paediatric cases that lasts for more than 8 weeks to be chronic, thus bringing it into line with chronic cough in adults.
At consultation, there is usually a disagreement between the symptoms and the subjective assessment of parents, i.e. their expectations. Parental smoking is a factor found in persistent cough in up to 50% of children under 11 years of age, with this value decreasing somewhat in adolescents.
The different aetiologies for each age group must be taken into account when managing chronic cough. Thus, for patients aged 14 years and younger, paediatric protocols will be used, whereas for adolescents aged 15 years or older, many authors recommend that adult protocols be used(7,9,10).
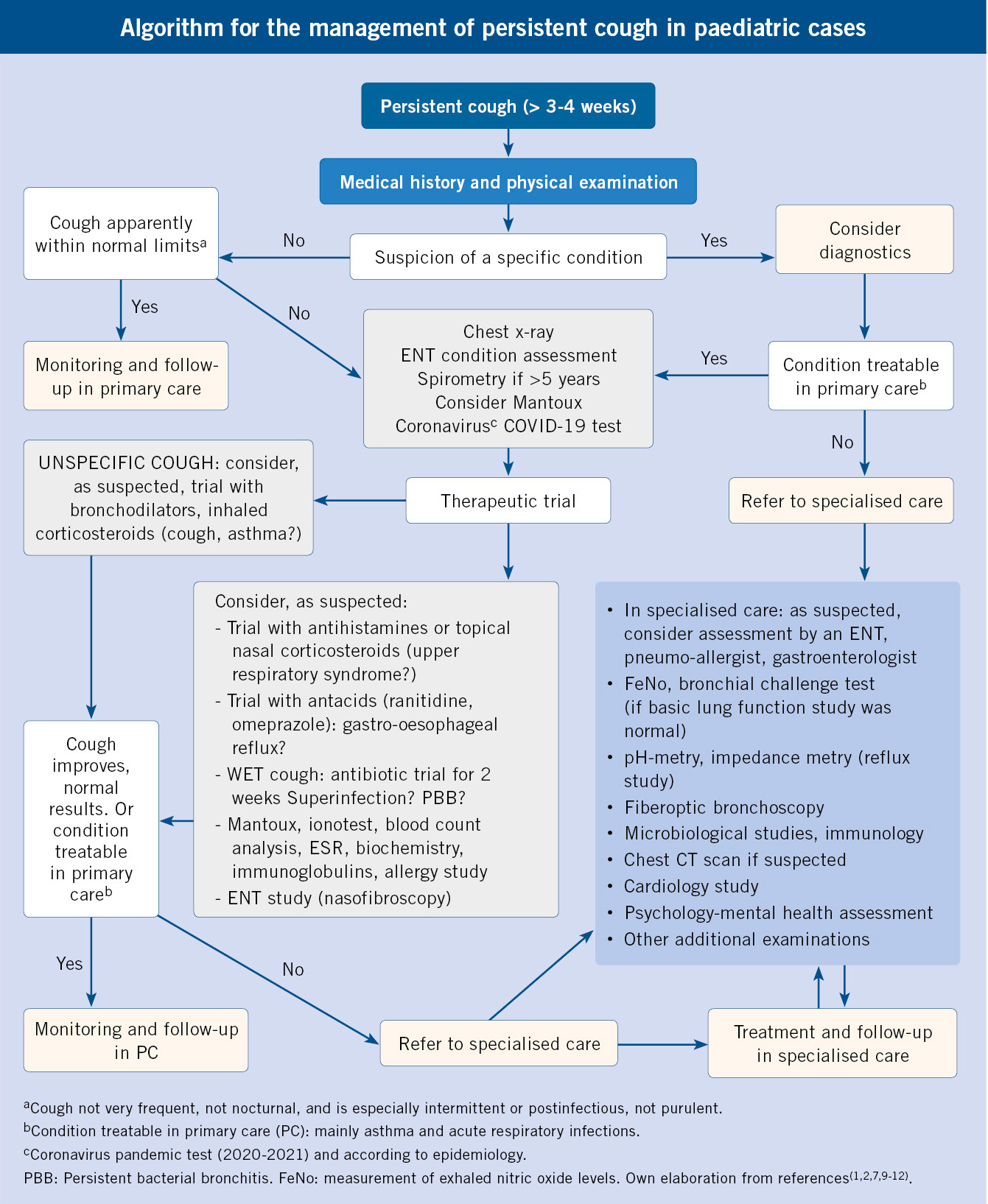
The use of algorithms must take into account the place of assessment, in other words primary care or specialised paediatric pneumology, and when implementing protocols, it is essential to have training which is especially aimed at recognising the specific aspects of cough and their clinical significance.
Aetiology
After assessing whether it is an expected cough or within normal limits and frequency, in prolonged cough we can consider two main groups:
• Specific cough: secondary to pulmonary and extra-pulmonary pathophysiological processes.
• Non-specific cough: with no apparent cause after an initial assessment(2,11,12).
From highest to lowest prevalence, in paediatric cases non-specific chronic cough usually has the following origin: post-infectious, cough as an asthmatic equivalent, psychogenic cough and chronic cough due to upper airway syndrome.
Isolated chronic cough without wheezing
This appears in apparently healthy children. Its causes include:
• Pulmonary abnormality or gastro-oesophageal reflux in infants.
• Cough as the only manifestation of asthma.
• Post-infectious cough.
• Respiratory infections: simple recurrent viral bronchitis or prolonged or pertusoid cough: Bordetella pertussis, Parapertussis, Mycoplasma, Chlamydia, Cytomegalovirus, Adenovirus, and Ureaplasma.
• In the current SARS Cov-2 or Covid-19 coronavirus pandemic, prolonged cough for more than one month is occasionally seen in paediatric cases(13). A study (Covid-19 PCR) is recommended in the event of an underlying disease or comorbidity and known contact with coronavirus.
• Rhinosinusitis. Allergic or not, which may or may not be associated with asthma.
• Psychogenic cough (somatic cough syndrome). Coughing habit (cough as a tic).
• Chronic upper airway cough syndrome (previously known as post-nasal drip syndrome).
Chronic cough in children with an underlying lung disease
• Cough as a manifestation of asthma.
• Gastro-oesophageal reflux, with or without aspiration.
• Persistent bacterial bronchitis (PBB).
• Chronic bronchitis: eosinophilic or not.
• Other diseases: tuberculosis, cystic fibrosis, foreign body aspiration, immunodeficiency, bronchopulmonary malformations, ciliary dysfunction, alpha-1-antitrypsin deficiency, tracheomalacia, obliterative bronchiolitis, chronic bronchitis, etc.
See Table I for the most frequent aetiology by age group.
Clinical Symptoms
The case history should be directed towards warning signs (neonatal age, association with general symptoms, aspiration and signs of suppurative bronchial inflammation), as well as by age, appearance, if the cough is dry or productive, and according to the epidemiological situation.
At consultation, questions about prolonged or chronic cough will be targeted(1,2,6) towards:
• Onset of the cough, age and whether or not it was associated with a respiratory infection.
• Characteristics of the cough: usual coughing style, to classify it as a dry or productive cough.
• If it is discontinuous, metallic, with stridor, paroxysmal, occurs regularly, is nocturnal or disappears during sleep, related to ingestion, has an abrupt onset, or is related to exercise or exertion (crying, laughing).
• If there is a possibility of distracting the cough or if there is a disproportionate concern about the cough. If it is related to: humidity, pets, smoke, environmental pollutants.
• Consideration should be given to: smoking, vaping (electronic cigarettes), use of inhaled drugs, use of irritants or chemical pollutants, such as hobbies (glues, paints) or in the workplace.
• Warning signs: onset in or near the neonatal period, or associated with general symptoms (weight loss, feeding difficulties, chronic diarrhoea, clubbing) or if there is haemoptysis.
• Other relevant information: fever, rhinorrhoea, catarrh, choking or aspiration of a foreign body, habitual vomiting, sputum production, risk of contact with tuberculosis or HIV, parental smoking, possible allergy and vaccination status.
• Personal history: prior diseases, especially pulmonary (pneumonia, congenital cardiopulmonary and autoimmune disorders, neoplasms, immunodeficiencies and medications). Where appropriate, geographic origin and possibility of endemic parasitic diseases: tuberculosis, histoplasmosis (USA), toxocara (China), echinococcosis (rural areas without adequate sanitary control).
• Previously performed additional examinations must be evaluated: chest X-rays or laboratory tests. Associated heart or neurological diseases or others, comorbidities (obesity, sleep apnoea, atopy). Also assess, where appropriate, what relieved the cough (inhaled corticosteroid, antibiotics, antihistamines)(1,2,6).
• When deciding treatment, it is important to take into account the impact on the child or adolescent’s quality of life in their various life environments, and it is necessary to enquire about this, as well as the parents’ expectations(5). In paediatric cases, there are multidimensional questionnaires (physical sphere, emotional and school and social functioning), such as the PedsQL or KIDSCREEN (kidscreen.org), which are recommended for use outside of research studies.
Complications
Complications due to chest-abdominal pressure caused by coughing, and due to the impact on social life, include: vomiting, petechiae, subconjunctival haemorrhage, cough syncope, urinary incontinence, musculo-skeletal pain, hoarseness, exhaustion, shyness, altered social relationships, insomnia, headache, dizziness, excessive perspiration, and concern that “something is wrong”, altered quality of life, lifestyle changes, abdominal hernias; and, less frequently: rib fractures (especially from 5th to 7th) induced by cough, pulmonary interstitial emphysema, pneumothorax, arrhythmias, etc.(1,2).
Diagnosis
This is based on a systematic clinical evaluation, with medical history and general physical examination. A first visit should be conducted to ask about: the existence of previous acute respiratory infections, the type of cough, the presence of signs of specific diseases and whether there are indicators of a specific cough or risk factors (infection, asthma, foreign body aspiration, etc.)(1,2,14).
This first visit, as well as the second assessment at 7-14 days, are key to initiating a diagnostic orientation and to consider additional targeted examinations.
Periodic reassessments and clinical control to determine the natural evolution or response to the initially targeted treatment are essential.
It should be remembered that prolonged coughing can improve spontaneously, thus overdiagnoses and unnecessary treatments should be avoided. In addition, at times, there may be two or more causes for the cough (e.g., asthma, rhinitis, persistent bacterial bronchitis, congenital airway abnormalities, and smoking).
Physical examination should be comprehensive, highlighting: weight/stature changes, skin colour, signs of atopy, thoracic deformity, clubbing, cardiopulmonary auscultation and a detailed examination of the pharynx, nose and ears, including the neck (explore the existence of goitre). Persistent auscultatory abnormality may be more associated with wet cough and other symptoms in addition to the cough(14,15)
Additional tests
In the diagnostic study for chronic cough, the different predominant aetiology according to age must be taken into account, and the diagnosis and targeted treatment for risk conditions must not be delayed. Paediatric protocols should be used for patients aged 14 years or younger.
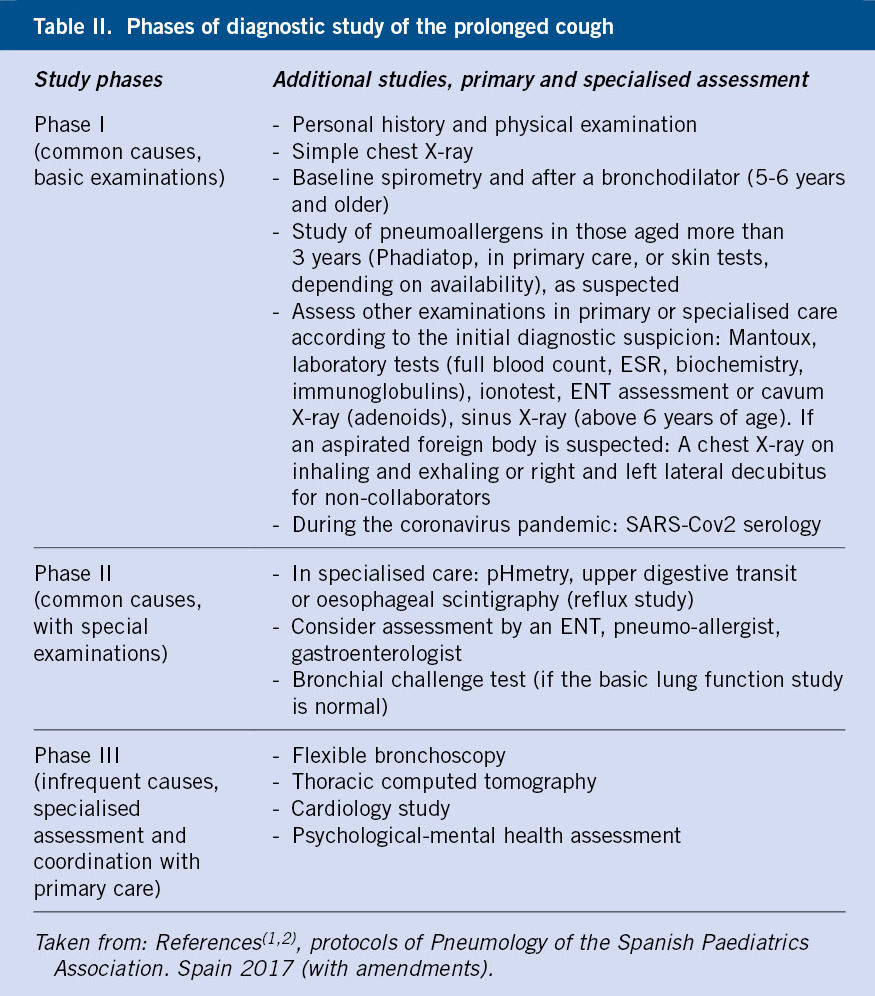
A sequential approach can be considered guided by: case history, physical examination, and by performing an x-ray and a forced spirometry. See table II for study phases or levels of prolonged cough and the management algorithm (7,9,10). In older children and adolescents, if there is a suspected diagnosis of rhinitis or cough as an expression of “postnasal drip”, an initial therapeutic trial in primary care could be initiated.
• Chest X-ray: a frontal projection is usually requested (AP up to 6 years, PA from that age onwards). In the event that the location of a lesion or imaging of the lung bases (e.g., with COVID-19) is required, two projections (PA and lateral) should be requested. This enables: asymmetries to be detected and congenital anomalies, radiopaque foreign bodies, infiltrates and atelectasis, increased cardiac silhouette to be seen. Other imaging studies depending on clinical suspicion: a sinus X-ray if sinupathy is suspected, ultrasound if the mediastinum is to be assessed, computed tomography can be useful if a more comprehensive study of the paranasal sinuses or alterations of the upper airway is desired, in the event of an altered chest X-ray or suspected lung disease. Magnetic resonance imaging will be useful in vascular disorders.
• Spirometry at baseline and after bronchodilation in collaborators and those older than 5-6 years (if within normal parameters, consider spirometry after treatment with inhaled or systemic corticosteroids). In the event of suspected asthma, the record of variability in peak expiratory flow or peak-flow and bronchoprovocation tests (this is only available in specialised centres) may reveal reversible obstruction and hyper-responsiveness, or suggest anatomical abnormalities (stenosis of the airways or malacia).
• Measurement of exhaled nitric oxide (FeNO) levels, available in specialised centres, which helps the diagnosis of eosinophilic asthma. The cut-off point generally proposed as pathological is 50 ppm. It has a high negative predictive value of up to 93%.
• Mantoux reaction. Tuberculosis screening could also be done with an IGRA (Interferon-Gamma Release Assay, such as Quantiferon)(16). Depending on the geographic area or risk of exposure, many physicians believe that tuberculin should be performed during the initial or first level assessment
• Study of allergies to aeroallergens in those aged 3-4 years and older, with a suspected diagnosis, perhaps more specifically for fungi or mites. Studies according to availability: in vivo test such as skin tests (“prick”), or in vitro (blood test) Phadiatop, Cap system (specific IgE in allergen groups) or similar, which are feasible in many primary care centres. The pneumoallergen profile, or specific IgE for individualised allergens, would be used. A negative Phadiatop indicates a very low probability of allergic sensitisation.
• Full blood count with ESR, basic biochemistry and TSH. In the event of a possible active infection. Goitre or thyroiditis may exceptionally be the cause of a cough as the only apparent initial symptom. During the SARS-Cov2 coronavirus pandemic, a serological study may be considered.
• Gastroesophageal reflux study. Reflux and chronic cough only coincide in 3-8% of paediatric cases; this is more common in infants, who do not usually manifest with cough alone, and in older children or adolescents, especially if there are other symptoms such as heartburn or regurgitation. A therapeutic trial with a proton pump inhibitor (e.g., omeprazole) for 8 weeks can be considered, and if there is no response, referral to a paediatric gastroenterologist, who may suggest: a digestive endoscopy, an oesophageal pH measurement if appropriate with double channel intra-luminal impedance or others (upper digestive tract or oesophageal scintigraphy). Achalasia has been described as a cause of chronic cough.
• Assessment by an ENT specialist. If chronic sinupathy or upper airway alteration is suspected. With nasofibroscopy, a diagnosis of turbinate hypertrophy with rhinitis and polyposis can be made.
• If sputum can be obtained, a gram and cultures are performed. And if available: the study of eosinophils and metachromatic cells in the induced sputum. This contributes to the diagnosis of asthma and eosinophilic inflammation of the airway.
• Serological tests: study of past viral infection, Mycoplasma pneumoniae, B pertussis, others.
• Determination of immunoglobulins and their classes, and other immunocompetence tests are suggested in cases of chronic infection. HIV infection study.
• Bronchoscopy. Rigid bronchoscope or fibre-optic bronchoscope. The indications are: extraction of a foreign body, in the event of congenital anomalies, to obtain samples from the lower airways (bronchoalveolar lavage [BAL]), for culture and microscopy. An increase in lipids in bronchoalveolar lavage may indicate microaspiration. Fibre-optic bronchoscopy with BAL for cytological study, culture and PCR, constitutes the definitive test for the diagnosis of persistent bacterial bronchitis, although its limited availability means that it is reserved for those patients with an insufficient response to antibiotic treatment or who present a recurring PBB (more than 3 episodes per year).
Tracheobronchomalacia and PBB are often related (48-74% of cases).
• The sweat test to rule out cystic fibrosis (CF) should be performed in the event of prolonged cough if there is malnutrition or a chronic productive cough. Over the past 11 years (since 2009), neonatal screening with immunoreactive trypsin in blood has become widespread in all of the Spanish territory. However, it must be considered that adolescents or migrants may not have undergone neonatal screening for CF.
• Primary ciliary dyskinesia is excluded only in specialised centres and requires in vivo and in vitro tests, electron microscopy and epithelial cultures. In the event of neonatal onset of cough, this should be considered in addition to situs inversus or congenital anomalies of the airway.
• In people with sickle cell disease, asthma can be a comorbidity that increases the severity of haemoglobinopathy; however, cough is not usually a sole symptom of complications.
Cough assessment in paediatric cases in primary care
It is important to assess whether cough is apparently normal or not, to consider the parents’ expectations, and to reassure most families. In the paediatric primary care consultation, in the presence of a child who is known, history taking of the characteristics of the cough, the presence of other signs of disease and the physical examination will likely guide us to suspect an underlying cause. Do not forget to consider persistent bacterial bronchitis as a non-uncommon cause of wet cough in children under 6 years of age. A chest X-ray should be performed, as well as additional examinations aimed at ruling out tuberculosis, coronavirus SARS-Cov 2, and spirometry in children aged more than 5 years.
The Phase I study and the left and central side of the algorithm should be used.
For appropriate treatment of prolonged cough in paediatric cases, an attempt should be made to clarify the cause, excluding serious underlying diseases. The presence of a long-standing cough should be investigated until it has fully disappeared or until a definitive diagnosis has been reached. Partial or temporary improvements in the cough should not be considered as a definitive therapeutic success. With an adequate approach, up to 80% of the causes of chronic cough in paediatric cases can be determined, and an improvement is seen in 90% of cases when treated(7,9-11,17).
Treatment
General measures
Oral hydration and nasal washes. Avoid exposure to tobacco and irritants.
Treatment with environmental measures
There is no evidence that home environmental management, including deionisers, vaporisers, humidifiers, air filters or others, are effective in the treatment of prolonged non-specific cough in paediatric cases.
Aetiological treatment
Once the cause is identified.
• Antibiotics for an established or suspected infection, for symptoms of PBB (2 weeks with amoxicillin-clavulanic acid at 80 mg/kg/day –adult dose, 875 mg amoxicillin/125 mg clavulanate–, as first choice), or cotrimoxazole, cephalosporins or macrolides (azithromycin 10 mg/kg/day, and up to 500 mg every 24 h, 3 days, or clarithromycin). Good response to antibiotic therapy also characterises and contributes to the diagnosis of PBB(12).
• Macrolides in the case of whooping cough (would not shorten the full-blown disease after 2 weeks of onset of the clinical coughing symptoms).
• For rhinitis or chronic cough syndrome of the upper airway, first-generation antihistamines due to their anticholinergic effect, or nasal corticosteroids.
• Treatment of allergic disease with environmental measures and inhaled steroids. For dry cough, the inhaled corticosteroid test for 4 weeks or leukotriene inhibitor (montelukast in those aged more than 6 months, as per the summary of product characteristics) as second option. If the anti-asthma treatment trial has failed, it must be discontinued.
• Surgical treatment for anatomical anomalies.
• Reflux can be treated medically (ranitidine in infants or omeprazole and lifestyles avoiding acidic drinks, colas, consumption immediately before bedtime, raised pillow), or surgically (Nissen fundoplication). In cases where there is no response to conservative treatment, chronic isolated cough will exceptionally be an indication for reflux surgery.
• Others: some authors have found a response to nebulised lidocaine for dry refractory cough in adults and children. In adults with chronic cough that does not respond to treatment, guanfacine or gabapentin have been used off-label (not indicated in the summary of product characteristics). Guanfacine is a selective alpha2A adrenergic receptor agonist, a centrally acting antihypertensive that is also approved for ADHD. Gabapentin is an anti-seizure drug that is also commonly used for the treatment of neuropathic pain.
Psychological support. Adequate information
For prolonged non-specific cough that is not indicative of any disease, it is important to inquire about the need for individualised information for the patient and family. Fears or prejudices may sometimes not be reported at first visits, and should be studied and properly addressed by counselling
The treatment for psychogenic cough (somatic cough syndrome) will be aimed at identifying the underlying conflict, reassuring parents and relatives, clearly explaining the benign nature of the process and not interrupting schooling. Relaxation techniques to decrease musculo-skeletal tension in the neck and chest can be successful. In extreme cases, refer to the psychiatrist and consider family hypnosis. Suggestion techniques may improve cough with a psychogenic origin: cough as a vicious circle triggered by irritants, which no longer works, concentrating on progressively spacing the cough, manoeuvres to relieve irritation, etc.(18).
Pharmacological cough treatment
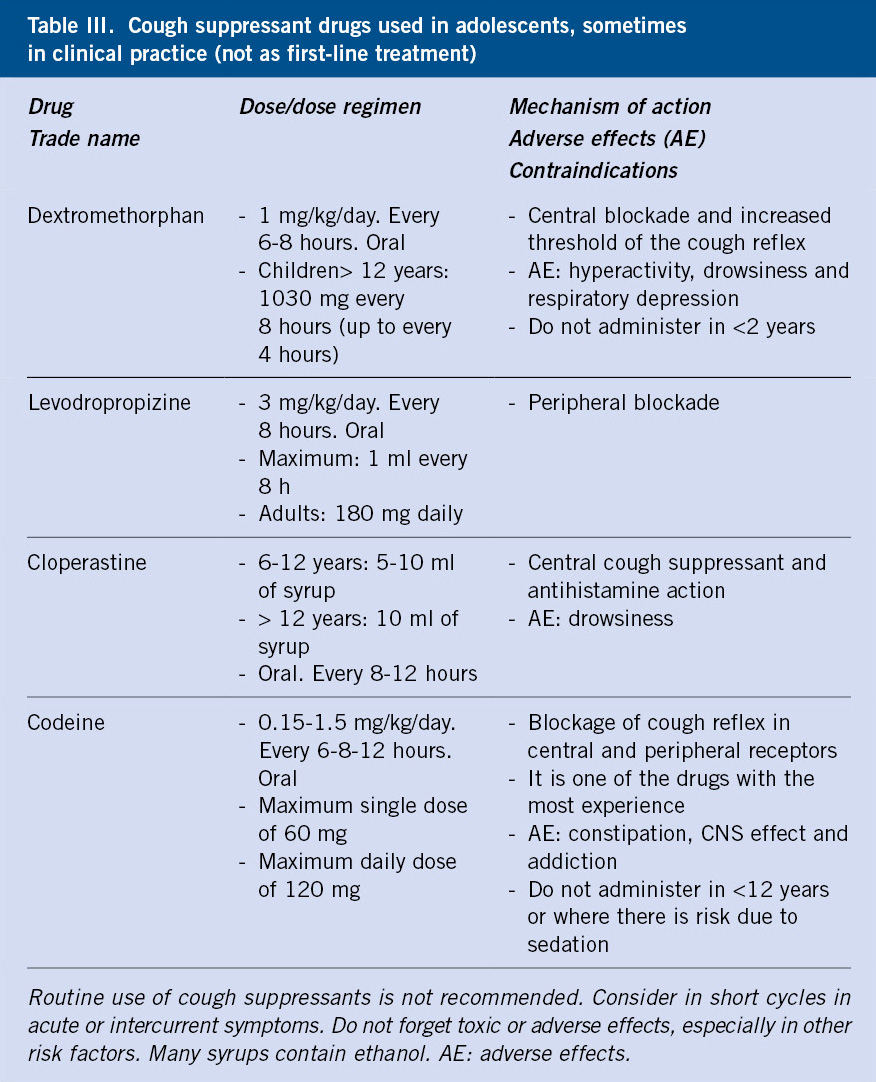
Cough suppressants should be used sparingly, in specific circumstances, never as first-line treatment and respecting the indications and contraindications according to age.
Cough suppressants are sometimes helpful for intractable cough, especially due to viral infections, but they should not be used as first-line treatment for prolonged cough as they can delay a specific diagnosis and its treatment. The most common cough-suppressant drugs in primary care are collected in Table III.
Adolescents and their parents should receive information about the drugs and their partial effectiveness, as well as the likelihood of adverse effects associated with their use. Codeine is the most important centrally, but since 2015 the Spanish Medicines Agency has recommended not to use codeine in children under 12 years of age, or in adolescents aged between 12 and 18 years who present compromised respiratory function of a pulmonary, neuromuscular, traumatic or surgical aetiology. There are also a variety of home remedies with a predominant placebo effect.
• Mucolytics, including bromhexine and acetylcysteine, should not be used for chronic cough as there is no evidence of efficacy and, in addition, they can cause irritation of the airway. Inhaled recombinant human DNase (alpha-dornase) may be effective in children with purulent viscous secretions and is indicated in cystic fibrosis.
• There are numerous current lines of research on new cough suppressants to act on the multiplicity of receptors or potential targets of the cough mechanism.
• For cough associated with treatment with antihypertensive angiotensin II inhibitors (ACEI), the latter must be suspended and, where appropriate, ARBs such as losartan or valsartan, which do not inhibit quinine metabolism, should be used. This is not common at a paediatric age.
Bibliography
The asterisks indicate the interest of the article in the authors’ opinion.
1.*** Pascual Sánchez MT, Urgelles Fajardo E. Tos persistente. Protoc diagn ter pediatr. 2017; 1: 1-14. Acceso el 26 septiembre de 2020. Available at: http://www.neumoped.org/docs/PROTOCOL_DIAGN_TERAP.pdf.
2.*** Chang AB, Marchant JM, Mallory GB, Hoppin AG. Approach to chronic cough in children. UpToDate 2020. Version October 2018. Accessed 26 October 2020.
3.* Kantar A, Seminara M, Why chronic cough in Children is different. Pulmonary Pharmacol Therapeut. 2019; 56; 51-6.
4. Mazzone SB, Undem BJ. Vagal afferent innervation of the airways in Health and Disease. Physiol Rev. 2016; 96: 975-1024.
5.* Newcombe PA, Sheffield JK, Petsky HL, Marchant JM, Willis C, Chang AB. A child chronic cough-specific quality of life measure: development and validation. Thorax. 2016; 71: 695-700.
6.** Zafra Anta MA. Tos crónica. En: Hidalgo Vicario MI, Rodríguez Molinero L, Muñoz Calvo MT. Eds. Medicina de la adolescencia. Atención integral. Majadahonda (Madrid): Ergón. 3ª ed; 2021. p. 585-90.
7.* Chang AB, Oppenheimer JJ, Weinberger M, Weir K, Rubin BK, Irwin RS. Use of management pathways or algorithms in children with chronic cough: Systematic reviews. Chest. 2016; 149: 106-19.
8.* Silvestri RC, Weinberger SE, Barnes PJ, King TE, Hollingsworth H. Evaluation of subacute and chronic cough in adults. UpToDate 2018. Version October 2018. Accessed 26 October 2020.
9.** Moneo Hernández I, Asensi Monzó M, Rodríguez Fernández-Oliva CR. Guía de Algoritmos en Pediatría de Atención Primaria. Tos crónica en AP. AEPap. 2017 (en línea). Consultado el 14 de noviembre de 2020. Available at: algoritmos.aepap.org.
10. O’Grady KAF, Grimwood K, Torzillo PJ, Rablin S, Lovie-Toon Y, Kaus M, et al. Effectiveness of a chronic cough management algorithm at the transitional stage from acute to chronic cough in children: a multicenter, nested, single-blind, randomised controlled trial. Lancet Chil Adolesc Health. 2019; 3: 889-98.
11.** Ridao Redondo M. Tos crónica en Pediatría. Pediatr Integral. 2016; XX(1): 7-15.
12.*** Busquets Monge RM, Castillo Corullón S, Aguilar Fernández AJ. Tos húmeda: bronquitis bacteriana persistente, enfermedad supurativa bronquial y bronquiectasias. Protoc diagn ter pediatr. 2017; 1: 15-29. Accessed 20 September 2020. Available at: http://www.neumoped.org/docs/PROTOCOL_DIAGN_TERAP.pdf.
13.** Devilla JG, Song E, Ouellette CP, Edwards MS, Torchia MM. Coronavirus Disease 2019 (COVID-19): clinical manifestations and diagnosis in Children. UptoDate 2020. Version november 2020. Accessed 12 november 2020.
14.* Zafra Anta MA. Semiología Respiratoria. Regreso a las Bases. Pediatr Integral. 2016; XX(1): 62.e1-62.e12.
15. Fernández Manso B, Albañil Ballesteros MR, Zafra Anta MA. Auscultación patológica persistente: no todo son broncoespasmos. Rev Pediatr Aten Primaria. 2019; 21: 173-9.
16. Zafra Anta MA, Rivero Calle I, García Begoña S. Tuberculosis (v.3/2020). En Guía-ABE. Infecciones en Pediatría. Guía rápida para la selección del tratamiento antimicrobiano empírico (en línea). Consultado el 3 de abril de 2020. Available at: https://www.guia-abe.es; https://guia-abe.es/files/pdf/Guia-ABE_Tuberculosis_v.3_2020.pdf.
17.** Seoane M, Sanz V, Villa JR. Tos crónica en la adolescencia. Adolescere. 2018; VI(3): 6-13.
18. Weinberger M, Lockshin B. When is cough functional, and how should it be treated? Breathe. 2017; 13: 22-30.
Recommended bibliography
– Pascual Sánchez MT, Urgelles Fajardo E. Tos persistente. Protoc diagn ter pediatr. 2017; 1: 1-14.
Article that summarises the fundamental characteristics and recommendations for the management of persistent cough in our environment, both in primary and specialised care.
– Chang AB, Marchant JM, Mallory GB, Hoppin AG. Approach to chronic cough in children. UpToDate 2020. Version October 2018.
Review with evidence-based medicine methodology of the clinical and epidemiological characteristics of prolonged cough, carried out by one of the leading international experts on the subject, which is constantly updated.
– Zafra Anta MA. Tos crónica. En: Hidalgo Vicario MI, Rodríguez Molinero L, Muñoz Calvo MT. Eds. Medicina de la adolescencia. Atención integral. Majadahonda (Madrid): Ergón. 3ª ed. 2021; p. 585-90.
Updated text specifically aimed at the 10-20 years age group.
– Moneo Hernández I, Asensi Monzó M, Rodríguez Fernández-Oliva CR. Guía de Algoritmos en Pediatría de Atención Primaria. Tos crónica en AP. AEPap. 2017 (on line). Available at: algoritmos.aepap.org.
Guide that serves as support and endorsement in the decision to carry out additional studies and referral where appropriate.
– Busquets Monge RM, Castillo Corullón S, Aguilar Fernández AJ. Tos húmeda: bronquitis bacteriana persistente, enfermedad supurativa bronquial y bronquiectasias. Protoc diagn ter pediatr. 2017; 1: 15-29.
Comprehensive analysis of chronic wet cough which is not as exceptional as one might think, and whose early treatment reduces the risk of chronic pulmonary complications.
– Chang AB, Oppenheimer JJ, Irwin RS; CHEST Expert Cough Panel. Managing Chronic Cough as a Symptom in Children and Management Algorithms: CHEST Guideline and Expert Panel Report. Chest. 2020; 158: 303-329.
Excellent review of the recent guidelines compared to the 2006 one with levels of evidence. It recommends following diagnostic guidelines by age. Diagnostic and treatment recommendations are presented.
– Morice AH, Millqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J. 2020; 55: 1901136 Available at: [https://doi.org/10.1183/13993003.01136-2019].
Chronic cough is recognised as a distinct entity. This European guide incorporates recent advances in pharmacological and non-pharmacological pathophysiology, diagnosis and the treatment of chronic cough.
Links of interest:
- GEMA Guide. Asthma management: https://www.gemasma.com/.
- Spanish Society of Paediatric Pneumology website: http://www.neumoped.org/.
- AEPap Respiratory Tract group: http://www.respirar.org/.
| Clinical case |
|
Tomás is 5 years old and visits primary care because, in the context of catarrhal symptoms, he started with a persistent wet cough more than 4 weeks ago. His parents report that he occasionally suffers from fatigue for a short time at the end of frequent coughing spells. He has no history of choking during a meal, or foreign body aspiration. There are no symptoms of Covid-19 in the family. There are no smokers in the home. He has not lost any weight. He has been in treatment for moderate asthma for two years with budesonide medium-dose chamber spray and montelukast. Upon examination he is afebrile, with disperse expiratory wheezing but no respiratory distress; the rest of the examination is normal. Treatment with salbutamol and an oral corticosteroid was initiated for 3 days, resulting in an improved auscultation but not the cough, which persisted. A chest X-ray was performed, with no findings reported. Poorly controlled asthma is considered and budesonide is replaced with a salmeterol-fluticasone spray with a chamber. There are no changes in the cough. Saturation with a finger pulse oximetry on several occasions is 96-99%. Oral amoxicillin-clavulanic acid was added to the treatment for 2 weeks, with improvement in the first 2-3 days, the cough disappearing and auscultation normalised.
|
 Persistent cough
Persistent cough