|
| Topics on Continuous Training |
J. Peralta Calvo
Consultant ophthalmologist. Ophthalmology Service, La Paz Children’s Hospital. Madrid. Associate Professor of Ophthalmology. Universidad Autónoma de Madrid
| Abstract
The most relevant ophthalmological emergencies for pediatricians in training and for those who practice in Primary Care are presented. The first section is dedicated to ocular and orbital trauma, with special attention to abusive head trauma (AHT) or “shaken baby syndrome”, management of ocular caustications and warning signs of orbital fractures. The second section includes inflammatory pathology, with emphasis on neonatal conjunctivitis (ophthalmia neonatorum) and the diagnosis and treatment of orbital cellulitis, including post-trauma etiology. Finally, the pediatrician must recognize the most relevant ocular oncological pathology, retinoblastoma, and make the differential diagnosis of leukocoria, the most important sign in pediatric ophthalmology. Rhabdomyosarcoma, the most prevalent malignant orbital tumor and its differential diagnosis with orbital cellulitis, is also presented. |
| Resumen
Presentamos las urgencias oftalmológicas de mayor relevancia para el pediatra en formación y el que realiza Atención Primaria. La primera sección se dedica a la traumatología ocular y orbitaria, con especial atención al trauma craneal abusivo (TCA) o “síndrome del niño zarandeado”, el manejo de las causticaciones oculares y los signos de alarma de las fracturas orbitarias. La segunda sección está comprendida por la patología inflamatoria, con hincapié en la conjuntivitis neonatal (oftalmia neonatorum) y el diagnóstico y tratamiento de las celulitis orbitarias, incluyendo las postraumáticas. Por último, el pediatra debe conocer la patología oncológica ocular más relevante, el retinoblastoma, y realizar el diagnóstico diferencial de la leucocoria, el signo más importante en Oftalmología pediátrica. Se expone también el rabdomiosarcoma, tumor orbitario maligno más prevalente y su diagnóstico diferencial con la celulitis orbitaria. |
Key words: Trauma; Caustication; Shaken; Retinoblastoma; Rhabdomyosarcoma.
Palabras clave: Traumatismo; Causticación; Zarandeo; Retinoblastoma; Rabdomiosarcoma.
Pediatr Integral 2023; XXVII (1): 41 – 47
OBJECTIVES
• To be able to identify closed globe trauma: lacerations and hyphema (intraocular bleeding), and suspect abusive head trauma (AHT) if certain indicators are present.
• To properly manage ocular caustications.
• To diagnose open globe trauma and to urgently manage it.
• To identify severe orbital fractures, orbital cellulitis and their differential diagnosis.
• To make the pediatrician aware of the importance of leukocoria, its clinical urgency and the rudiments of differential diagnosis.
• To recognize the existence of rhabdomyosarcoma as the most frequent malignant orbital tumor, and its differential diagnosis with cellulitis.
 |
 |
Ophthalmological emergencies
Introduction
Emergencies in pediatric ophthalmology cover different etiologies, which can affect different ocular structures.
I have divided the topics according to the main etiologies, and I have subdivided them according to the altered structure and the most prevalent symptoms in the practice. The objective is that all pediatricians recognize what the different urgent ophthalmological syndromes are and their basic management.
Ocular trauma
Pediatric eye injuries account for up to 35 % of all injuries reported in the US(1) and may require hospital admission in 8.85-15.2/100,000 children per year(2).
Most injuries take place at home, particularly in younger children, so they could be largely preventable. A male prevalence has been documented throughout the literature, which intensifies with age, in the same way that sport causes predominate with age. On the other hand, the pediatric patient is susceptible to a particular type of “non-accidental” trauma, the “shaken baby syndrome” (SBS), more frequent in children under three years of age.
It is important to divide ocular globe trauma into two main types, depending on whether or not the outer covering of the eye, made up of the cornea and sclera, has been fully preserved in its entire thickness: closed and open.
Closed globe trauma
Eye contusions
They mainly manifest by bleeding in the anterior chamber, called hyphema(3).
The deformation of the eyeball by a contusion on its anterior pole (for example, if hit by a ball), causes tears in the iris vasculature, with a consequent hemorrhage, which tends to deposit in the lower area of the anterior chamber (space between cornea and iris). It can be observed up close with the help of a flashlight, as a reddish level in the lower part of the iris (Fig. 1). Hyphema can coincide with other eye injuries, especially eye opening, which must be ruled out in the emergency room.
Figure 1. Hyphema is visualized as a reddish level in the lower part of the anterior chamber (partially hiding the iris).
Hyphema can complicate, typically producing blood staining of the cornea, which is irreversible. Blood impregnation of the cornea is more frequent in large hyphema and/or with associated ocular hypertension. Both situations are more frequent if there is rebleeding, a phenomenon that tends to occur between the 3rd and 5th day. Traditionally, pediatric patients with hyphema have been admitted in order to restrict their mobility and closely monitor possible rebleeding, although this practice is currently out of use. Topical mydriatic, anti-inflammatory, and ocular hypotensive medication (if necessary) are prescribed, along with bed rest with the head raised by two pillows and movement restriction. In certain severe cases, the patient is admitted and fibrinolysis inhibitors are added to delay clot retraction and prevent rebleeding.
On the other hand, one must remember that spontaneous hyphema can occur in retinoblastoma. All spontaneous hyphema is suspicious of retinoblastoma until proven otherwise. Also, hyphema is the typical ocular presentation of juvenile xanthogranuloma.
Pediatrician’s attitude: both traumatic and spontaneous hyphema must be referred to the ophthalmologist on call.
Trauma erosions-ulcers on the cornea and conjunctiva
They are visualized with fluorescein staining (there is a commercial brand that mixes a topical anesthetic with fluorescein) and a cobalt filter in the flashlight, which produces a greenish fluorescence in the eroded area.
They may accompany the contusion and present with hyphema.
Pediatrician’s attitude: treatment of a trauma ulcer can be started if its diagnosis is certain and if the ulceration is not superinfected. Treatment consists of prevention of infection with antibiotic eye drops every 8 hours and cycloplegia if there is a lot of pain (e.g., cyclopentolate eye drops every 8 hours). In most cases, the eye is occluded in order to avoid manipulation and restrict blinking over the ulcer.
Non-accidental trauma
Traditionally called “shaken baby syndrome” (SBS), today the term “abusive head trauma” (AHT) is recommended, which is less restrictive(4), since shaking is not always present as the mechanism of the injuries.
The typical triad consists of: subdural hematoma, encephalopathy, and retinal hemorrhages. It is an entity that affects children under 3 years of age, with an incidence of up to 30 cases per 100,000 children in the US per year(5). It can cover shaking, impacts and other forms of abuse. It is linked to incoercible crying crises. There is no proven pathophysiological explanation of how shaking causes retinal hemorrhages, although it may be due to sudden retinal venous hyperpressure due to increased intracranial or thoracic venous pressure, and/or movement of the vitreous humor within the eyeball.
Every pediatrician should consider the possibility of non-accidental trauma, especially when the history reported by parents or caregivers is not consistent with the child’s condition.
It is not always easy to arrive at this suspected diagnosis(6), but there are certain “red flags”, such as: irritability, lethargy, obnubilation, respiratory distress, vomiting, malnutrition or multiple fractures (especially diaphyseal and/or in different stages of healing). Radiology is very useful in detecting fractures and intracranial bleeding. Retinal hemorrhages are present in 80 % of cases, and must always be ruled out. The ophthalmologist will confirm the presence of retinal hemorrhages and if these are suggestive of abuse: very numerous, bilateral, in different layers of the retina or preferably pre-retinal (in “dome”) and predominantly central (macular) hemorrhages (Fig. 2). The severity of hemorrhages correlates with the severity of brain damage. Poor visual acuity at diagnosis also indicates brain damage, with a poor vital prognosis. Visual limitations in survivors (approximately 70 %) are mainly of cerebral origin(7), due to a hypoxic-ischemic mechanism.
Figure 2. Several retinal hemorrhages are seen in a case of abusive head trauma, the largest in the macular area (in “dome”).
Chemical burns (caustications)
They are produced by the contact of certain chemical products on the ocular surface, normally with associated eyelid involvement.
Alkalis (e.g.: lime, caustic soda, bleach-sodium hypochlorite and ammonia) are more frequent and destructive, since they have greater ocular penetration. Chemical burns destroy the glands on the ocular surface, preventing the generation of tears, essential for corneal function. In addition, they damage a fundamental structure, the sclerocorneal limbus, where the stem cells that regenerate the corneal epithelium reside. If the limbus is damaged, corneal transparency will be lost. Chemical burns are still a significant problem, affecting more children in developing countries(8).
Pediatrician’s attitude: if you are faced with ocular caustication, you should irrigate the ocular surface copiously with physiological saline, to drag and dissolve the poison as soon as possible. You must evert the upper eyelids to clean the solid remains of the substance that have become adhered. You can check the pH of the ocular surface using urine test strips. Subsequently, the patient should be referred to the ophthalmologist on call, as soon as possible.
Open eye globe trauma
Together with burns, they are the most serious, since they involve intraocular structures, in addition to the associated risk of infection (endophthalmitis).
Nowadays, there are visual prognostic systems(9) that calculate the probability of suffering legal blindness according to visual acuity at diagnosis, the type of trauma, whether there is endophthalmitis, retinal detachment or an afferent pupillary defect (no reaction of both pupils to light over the affected eye).
Open ocular trauma usually produces visible changes in the appearance of the globe: it can be deformed by leaking intraocular fluid (aqueous or vitreous humor), with subconjunctival hemorrhages (Fig. 3), pupillary deformation or prolapse of intraocular content (iris or ciliary body more frequently). Sometimes, the child reports that his eye “cries”, tears that are due to the leakage of aqueous humor from the wound.
Figure 3. Open globe trauma (ocular “bursting”). Subconjunctival hemorrhages with deformation of the eyeball.
Pediatrician’s attitude: upon suspicion of an open ocular trauma, the pediatrician will try to have as little manipulation as possible on the globe, to avoid the loss of intraocular contents. A protective plastic shield is recommended. He will leave the child fasting and request a preoperative period, since the child will be operated on urgently.
The pediatrician can confirm an ocular perforation in cooperative children using the Seidel test: if fluorescein eye drops are placed on the ocular surface and illuminated with blue light, the fluorescein will be washed from the ocular surface by the discharge of aqueous humor from the wound. It is a non-invasive test.
Orbital trauma
Orbital fractures
Orbital fractures are caused by violent contusions that transmit great energy to the orbit, fracturing at the points of least resistance, which are the papyraceous lamina of the ethmoid and the orbital floor (“blow-out”).
In both situations, the paranasal sinus is in contact with the orbit, facilitating the passage of air into it (pneumoorbit). The air is appreciable by crepitus on palpation, and increases with forced expiration maneuvers. From a clinical point of view, fractures of the orbital floor are more important, for two reasons: first, the inferior rectus muscle can become embedded in the fracture, producing a restrictive squint, with diplopia; second, part of the orbital content can prolapse into the maxillary sinus: the globe will appear sunken (enophthalmos).
Orbital fractures have a particularity in children: they can be “green stick”, that is, “trapdoor” type. After the fracture, the bone fragments return to their place, as if nothing had happened, but they trap orbital content, especially the inferior rectus muscle(10). This causes the triggering of the oculocardiac reflex when attempting to move the eye, which is manifested by nausea, vomiting, bradycardia, and syncope. It is a vagal reflex that is released when manipulating an extraocular muscle, as occurs in strabismus surgery.
Typically, there are very few external signs of the contusion (“white eye”) and its radiological visualization is difficult, even on CT scan. It is considered an emergency. The rest of orbital fractures, even in children, are subjected to a two-week observation period. Surgery is performed if diplopia or significant enophthalmos persists.
Pediatrician’s attitude: the existence of a fracture of the orbital floor should be suspected in the event of a contusion with subsequent ocular motility problems. The patient should be referred to the ophthalmologist on call, especially urgently if the child presents vagal phenomena.
Intraorbital foreign bodies
Children may present in the emergency room with intraorbital foreign bodies, frequently in a delayed manner.
On many occasions, parents do not report a previous trauma (because it has occurred without their supervision) or have not given it any importance. They come when they already notice inflammation of the eyelids or changes in the child’s condition. The typical example of this type of this trauma involves the pencil(11): after minimal eyelid penetration, important structures may be injured and/or fragments of wood or graphite remain retained in the orbit. Pens can easily reach the cavernous sinus. Also, the possible infection and inflammatory reaction that accompanies the fragments of wood and graphite must be considered. The result is severe orbital inflammation, with the possibility of intracranial extension and severe neurological involvement. Treatment should be early and surgical, although a careful radiological study is mandatory to locate the material and identify accompanying vascular involvement.
Pediatrician’s attitude: in the event of atypical palpebral lesions, compatible with lacerations, information should be obtained on the possibility of trauma, bearing in mind the possibility of toys and pens. If, after an eyelid laceration, the child presents changes in behavior, lethargy, malaise, or vomiting, the possibility of a retained orbital foreign body should be considered, with CT being the best diagnostic option. If the child presents clear signs of orbital cellulitis, and in the context of a laceration, an initial CT scan is indicated. In any case, post-trauma cellulitis will require hospital admission for broad-spectrum intravenous antibiotic treatment.
Inflammatory pathology
The emergencies of inflammatory origin that the pediatrician should be aware of are newborn conjunctivitis and orbital cellulitis.
Ophthalmia neonatorum
It is an entity still present in our population. It refers to newborn conjunctivitis, acquired in the birth canal, and every pediatrician should know about it.
The following etiologies conform it(12):
• Gonococcal conjunctivitis: it is the most severe, since Neisseria can perforate the cornea. It starts early (before the 5th day) and presents with a purulent and bloody discharge. Diagnosis will require Gram stain and culture, however it is not necessary to await for the results: a 125-mg dose of ceftriaxone is injected intramuscularly. Topical treatment is secondary, hygiene with physiological saline is sufficient.
• Chlamydial conjunctivitis (Chlamydia trachomatis): it is the most frequent nowadays. It presents a delayed onset, beyond the first week (although early rupture of membranes can anticipate presentation). The discharge is mucopurulent, not as severe as in gonococcal infections, and causes scarring of the cornea, as well as possible extension to the respiratory system. Definitive diagnosis is currently made by PCR. Treatment will consist of oral macrolides for two weeks. They can be associated topically.
• Herpes conjunctivitis keratitis: It also presents with a late onset, in the second week. Conjunctivitis is follicular, reminiscent of adenovirus, and can present dendritic corneal lesions and skin vesicles. The virus can cause retinal and neurological involvement. The definitive diagnosis is made by PCR. Treatment is oral acyclovir for two weeks.
• Conjunctivitis in relation to dacryostenosis (congenital obstruction of the nasolacrimal duct): these conjunctivitis tend to occur later, the origin being the accumulation of debris on the ocular surface due to lack of tear drainage to the nose. Various antibiotic eye drops can be used, mostly with aminoglycosides, and hydrostatic lacrimal massage after instillation is recommended to parents.
Pediatrician’s attitude: the pediatrician is involved in the prophylaxis of this pathology, recommending the instillation of erythromycin(13) ointment in the newborn’s eyes. When faced with a newborn with discharge, the pediatrician can take samples and begin treatment guided by the clinical picture; although it is prudent to promptly refer the patient to the ophthalmologist on call.
Orbital cellulitis
Orbital cellulitis is a frequent cause of emergency room visits and is much more frequent in children(14).
The most prevalent form is preseptal, that is, the involvement of the eyelids without affecting the orbit itself. It consists of a uni or bipalpebral swelling with erythema. The child will present fever and leukocytosis. The origin usually lies in the paranasal sinuses, and more frequently the ethmoid, due to contiguity. Other less frequent causes are bites, trauma (as previously mentioned) and teeth. These cases are usually more serious, due to more aggressive germs (anaerobes, S. pyogenes). A special form of cellulitis that complicates trauma is necrotizing fasciitis, frequently caused by S. pyogenes, which is characterized by a rapid progression towards gangrene, and which requires surgical debridement(15).
On the other hand, in its progression, preseptal cellulitis can be complicated by orbital cellulitis, orbital abscess and cavernous sinus thrombosis. All these complications are severe and require hospital admission. Orbital cellulitis is distinguished from preseptal cellulitis by proptosis of the globe (it appears propelled forward in the orbit), with extraocular motility difficulties. If it continues to evolve, it may present visual loss due to compression of the optic nerve and/or ocular vasculature.
Microbiology of cellulitis has changed since the generalization of the anti-Haemophilus vaccine in the 1990s. Currently, there is a higher prevalence of Gram-positive germs (pneumococci, staphylococci and streptococci), with a gradual increase in methicillin-resistant staphylococci.
Certain large retinoblastomas, with intense tumor necrosis, can produce orbital cellulitis due to the release of TNF (Tumor Necrosis Factor), without there being an extraocular extension of the tumor. These eyes usually present other signs of retinoblastoma, such as leukocoria or previous strabismus (Fig. 4).
Figure 4. Orbital cellulitis of tumor origin. Leukocoria (retinoblastoma) is seen.
Pediatrician’s attitude: the pediatrician in both Primary Care and the emergency room can treat preseptal cellulitis. Orbital extension must be ruled out by clinical examination. In doubtful cases or when there is suspicion of an extrasinusal origin, a CT scan should be performed. Treatment in uncomplicated forms will consist of a broad-spectrum antibiotic, such as high-dose amoxicillin-clavulanic acid, or third-generation cephalosporins.
Tumor pathology
Malignant tumor pathology is an emergency to the extent that the delay in diagnosis can condition the treatment of the child and his survival in the most severe cases. Retinoblastoma and rhabdomyosarcoma will now be discussed.
Retinoblastoma
Retinoblastoma is the most common intraocular tumor in childhood, with an estimated incidence of around 1/17,000 live births(16).
It originates in the precursors of the photoreceptors (cones) and has a widely known genetic cause: the inactivation of the two alleles of the RB1 gene, which encodes a protein involved in cell cycle arrest. Without this protein the cell begins mitosis. It is estimated that between 25 and 33 % of retinoblastomas have a germline mutation, that is, in all the cells of their body. These children therefore have a general predisposition to tumorigenesis. They have multiple (multifocal) retinoblastomas and are usually bilateral. In addition, they can develop tumors in the central nervous system, especially in the pineal gland (third tumor), and they can also develop other cancers throughout their lives, especially bone sarcomas and skin tumors.
RB1 germline mutators are usually spontaneous (“de novo”, the first case that occurs in the family), although we know of affected families (about 15 % of germline mutators). Most retinoblastomas are sporadic: a single precursor retinal cell loses both RB1 alleles (somatic mutations). Predictably, these tumors develop later than germline mutators (2 years vs. 9 months). Sporadic retinoblastomas are unilateral and single tumors.
The most common reason for consultation in retinoblastoma is leukocoria (Fig. 5), followed by strabismus.
Figure 5. Example of leukocoria. This is the same patient as in the previous figure, after starting systemic corticosteroid therapy.
Often, it presents with both signs. Leukocoria (“white pupil”, “white pupil reflex”) due to retinoblastoma originates from two main causes: on the one hand, it can be caused by a retinal detachment; on the other hand, it may be caused by the typical whitish color of the tumor, which is enhanced by the numerous calcifications that it normally presents. Strabismus occurs when there is the central area of the retina, the macula lutea, is affected, which provides maximum visual acuity.
Like all malignant tumors, retinoblastoma worsens over time, presenting more advanced grades in the classification used today, the International Classification of Retinoblastoma. This classification predicts the response to chemotherapy, the most widely used treatment nowadays, both systemic and local (intraarterial and/or intravitreal). The response to treatment is lower in the advanced grades. Hence the importance of an early diagnosis.
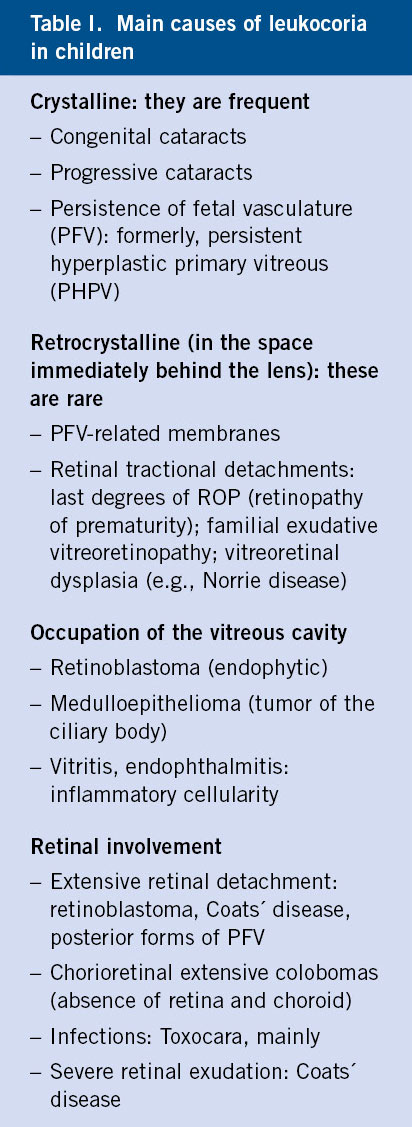
Leukocoria forces us to make a differential diagnosis that rules out the presence of retinoblastoma (Table I).
The most common cause of leukocoria in our setting is congenital cataract, especially bilateral. In younger children, persistence of the fetal vasculature (PFV) is the pathology that is most often confused with retinoblastoma(17). PFV, previously called persistent hyperplastic primary vitreous, is an abnormality of ocular development, closely linked to the lack of involution of the hyaloid vascular system, present in the embryo and in the fetus, and which runs through the entire vitreous cavity from the papilla of the optic nerve to the lens. Eyes with PFV are smaller and can present abnormalities in practically all structures, especially in the lens (cataracts and retrolental membranes) and in the retina (tractional detachments). In children older than 2 years, it is Coats´ disease that is most often confused with retinoblastoma. Coats’ disease is due to the existence of retinal telangiectasias (dilation of the venules) normally peripheral. These telangiectasias are incompetent, exuding plasmatic material into and under the adjacent retina(18). The exudation is yellowish in color due to the lipids it contains and gives the retina a yellowish discoloration. If the retina detaches, which occurs in the natural history of Coats’ disease, it will enter the differential diagnosis of leukocoria.
Pediatrician’s attitude: leukocoria is a highly relevant clinical sign, since it may be due to retinoblastoma. Parents may refer to the pediatrician that the child “has been looking in a strange way” for some time. This “weird look” is the most common way parents refer to leukocoria today. Some may comment that they have seen a “strange reflex in the eye”, or that the child’s eyes come out differently (from each other) in the photos. All these expressions are equivalent to the same thing: leukocoria.
The pediatrician must be aware that leukocoria is a possibility and must always rule out its presence in subsequent check-ups of the child.
When examining the eyes it is necessary to stop at the assessment of the pupil. It is better to carry out this assessment in semi-dark conditions, since the pupil is larger in this way, as the photomotor reflex decreases. With a flashlight we can check the photomotor reaction of each pupil, while we observe its color. At this time, we can already verify the whitish discoloration in the pupillary area, especially the presence of cataracts.
Immediately afterwards, we will practice the pupillary red reflex test. To do this, we take the direct ophthalmoscope and focus each eye separately from a distance between 33 and 50 cm. The beam of light projected by the ophthalmoscope is reflected on the retina, giving a reddish hue to the pupillary area. In order to better focus the pupillary plane, we must introduce lenses of +1 or +2 diopters in the ophthalmoscope system (when we turn the disk, we see that a value changes in a numeric indicator on the front: the red numbers are equivalent to diverging [negative] lenses, while blacks are converging [positive] lenses). If the reflection is whitish, we will speak of leukocoria. We must always compare the reflection of both eyes. In fact, the test can be performed simultaneously (Brückner test), for which we must move away from the child up to 66-100 cm. The reflection of the fundus of the eye (retina) negatively highlights the lens opacities, which appear black on the red background. These tests were recommended by the American Academy of Pediatrics for eye screening in children(19). Scans are greatly facilitated with pupillary dilation. Pupillary dilation is a safe procedure. Just one drop of 1 % cyclopentolate eye drops (0.5 % if under one year old) in each eye, which can be repeated after 10 minutes. The examination can be carried out half an hour after the first instillation.
At the end of a correct examination, we may diagnose leukocoria or, at least, its suspicion. Leukocoria is a reason for urgent hospital referral. If it is a retinoblastoma, chemotherapy can be started as soon as possible. In cataracts, PFV, and Coats’ disease, the functional outcome is coupled with early treatment.
Rhabdomyosarcoma
It is the most common soft tissue sarcoma in children and the most common malignant orbital tumor in childhood. Due to its aggressiveness it is frequently confused with cellulite.
It has a peak incidence around 7 years of age. It is a tumor that is not related to the extraocular muscles, despite the fact that it originates from precursors of striated muscle fibers.
The tumor is fast growing, especially in younger children. It tends to be located in the upper region(20), so it can present with palpebral ptosis (drooping of the upper eyelid). Normally, there is a proptosis (protrusion of the eyeball) with eccentric displacement of the eye, together with inflammatory signs that simulate conjunctivitis or cellulitis (Fig. 6). In many cases there is a visible lump or tumor. Pain is not usually present.
Figure 6.
For its diagnosis, MRI is essential, which shows certain characteristics in the sequences. MRI also allows differential diagnosis with cellulitis and with other tumors.
The tumor that can most frequently be confused with rhabdomyosarcoma is orbital lymphangioma, a benign tumor of venous-lymphatic lineage, characterized by intralesional bleeding crises, with accompanying proptosis. Cysts with blood levels, pathognomonic of this tumor, typically appear on MRI.
The treatment of rhabdomyosarcoma involves an excisional biopsy (which obtains as much of the tumor as possible, without injuring functionally important structures). Once the diagnosis has been obtained and staging has been carried out, aggressive intravenous chemotherapy is indicated, followed by radiotherapy according to the American protocols. The European protocol reserves radiotherapy for recurrences after chemotherapy.
Pediatrician’s attitude: the management of orbital cellulitis has already been discussed, which requires, on numerous occasions, a CT scan. This may be the path of diagnosis of an orbital tumor. Any rapidly growing tumor should be referred to the ophthalmologist on call, even if it only affects the eyelid.
Role of the primary care pediatrician
The Primary Care pediatrician must recognize the severity of an ocular trauma, and the indication for referral to the hospital emergency room. This physician can diagnose and treat corneal erosion, identify hyphema and open eye trauma. She/he can suspect a case of child abuse based on the clinical picture and refer to the ophthalmologist for confirmation. In case of causticization first aid must be applied. In the face of apparently trivial orbital trauma, muscular involvement in the orbital floor should be suspected due to vagal reactions, as well as retained orbital bodies due to inflammatory symptoms and/or systemic involvement.
In the case of ophthalmia neonatorum, there is clinical evidence to guide treatment, before receiving microbiological confirmation. In orbital cellulitis the differential diagnosis with tumors must be made: both retinoblastoma and rhabdomyosarcoma, which can cause orbital inflammation. The pediatrician is trained to initiate treatment in mild preseptal cellulitis.
Every doctor should be aware of the importance of leukocoria as a sign, and approach it as an emergency. This professional can even rule out certain causes, such as congenital cataracts, through observation without equipment.
Conflict of interest
There is no conflict of interest in the preparation of the manuscript. Declaration of interests: none.
Bibliography
The asterisks reflect the interest of the article in the opinion of the author.
1. Brophy M, Sinclair SA, Hostetler SG, Xiang H. Pediatric eye injury-related hospitalizations in the United States. Pediatrics. 2006; 117: 1263-71.
2.** Abbott J, Shah P. The epidemiology and etiology of pediatric ocular trauma. Surv Ophthalmol. 2013; 58: 476-85.
3. Crouch ER Jr, Crouch ER. Management of traumatic hyphema: therapeutic options. J Pediatr Ophthalmol Strabismus. 1999; 36: 238-50.
4. Christian CW, Block R; Committee on Child Abuse and Neglect; American Academy of Pediatrics. Abusive head trauma in infants and children. Pediatrics. 2009; 123: 1409-11.
5.** Mungan NK. Update on shaken baby syndrome: Ophthalmology. Curr Opin Ophthalmol. 2007; 18: 392-7.
6. Maiese A, Iannaccone F, Scatena A, Del Fante Z, Oliva A, Frati P, et al. Pediatric abusive head trauma: A systematic review. Diagnostics. 2021; 11: 734.
7. Kivlin JD, Simons KB, Lazoritz S, Ruttum MS. Shaken baby syndrome. Ophthalmology. 2000; 107: 1246-54.
8. Ahmmed AA, Ting DSJ, Figueiredo FC. Epidemiology, economic and humanistic burdens of ocular surface chemical injury: A narrative review. Ocul Surf. 2021; 20: 199-211.
9.** Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002; 15: 163-5.
10. Chung SY, Langer PD. Pediatric orbital blowout fractures. Curr Opin Ophthalmol. 2017; 28: 470-6.
11. Cho WK, Ko AC, Eatamadi H, Al-Ali A, Abboud JP, Kikkawa DO, et al. Orbital and orbitocranial trauma from pencil fragments: role of timely diagnosis and management. Am J Ophthalmol. 2017; 180: 46-54.
12.** Mallika P, Asok T, Faisal H, Aziz S, Tan A, Intan G. Neonatal conjunctivitis – a review. Malays Fam Physician. 2008; 3: 77-81.
13. US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, et al. Ocular prophylaxis for gonococcal ophthalmia neonatorum: US Preventive Services Task Force Reaffirmation Recommendation Statement. JAMA. 2019; 321: 394-8.
14. Tsirouki T, Dastiridou AI, Ibánez Flores N, Cerpa JC, Moschos MM, Brazitikos P, et al. Orbital cellulitis. Surv Ophthalmol. 2018; 63: 534-53.
15. Proia AD. Periocular necrotizing fasciitis in an infant. Surv Ophthalmol. 2018; 63: 251-6.
16.*** Munier FL, Beck-Popovic M, Chantada GL, Cobrinik D, Kivelä TT, Lohmann D, et al. Conservative management of retinoblastoma: Challenging orthodoxy without compromising the state of metastatic grace. “Alive, with good vision and no comorbidity”. Prog Retin Eye Res. 2019; 73: 100764.
17. Goldberg MF. Persistent fetal vasculature (PFV): an integrated interpretation of signs and symptoms associated with persistent hyperplastic primary vitreous (PHPV). Am J Ophthalmol. 1997; 124: 587-626.
18. Shields JA, Shields CL, Honavar SG, Demirci H, Cater J. Classification and management of Coats disease: the 2000 Proctor Lecture. Am J Ophthalmol. 2001; 131: 572-83.
19.*** Committee on Practice and Ambulatory Medicine Section on Ophthalmology; American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. Eye examination in infants, children, and young adults by pediatricians: organizational principles to guide and define the child health care system and/or improve the health of all children. Ophthalmology. 2003; 110: 860-5.
20.** Shields JA, Shields CL. Rhabdomyosarcoma: review for the ophthalmologist. Surv Ophthalmol. 2003; 48: 39-57.
21. Martín Gómez V, Casanovas Gordó JM. Traumatismos oculares. (Eye trauma) Pediatr Integral 2018; XXII: 45-57.
Recommended bibliography
– Lambert SR, Lyons CJ.Taylor & Hoyt’s pediatric ophthalmology and strabismus. 5th ed. London: Elsevier; 2017.
A reference book in pediatric ophthalmology. It addresses the entire subject, including the differential diagnosis of leukocoria, orbital cellulitis and ophthalmia neonatorum.
– Kuhn F, Pieramici DJ. Ocular trauma. Principles and practice. New York. Thieme; 2002.
It contains all ocular trauma in short chapters, including a specific one on the pediatric patient. It contains references to classification, emergency evaluation and medical-legal aspects, among others.
| Clinical case |
|
Reason for consultation: a 7-month-old infant is brought by his mother to the Health Care Center, after falling from the crib. History: the mother reports that the child has fallen out of the crib in an oversight and that she believes that he may have hurt himself. The crib has an approximate height of 1 meter. Personal history: the patient has no previous history of interest. The mother does not report any other significant events. Examination: the child is sleepy, with little contact with the outside world and barely smiling. There are some bruises on his buttocks and abrasions on his arms. Palpation of the right arm is painful, and a roughness over the humerus can be seen. Weight is in the 5 % percentile, as is the height percentile. Complementary tests: on the anteroposterior X-ray of the arm, a fracture line appears in the diaphysis of the humerus, which does not seem recent. Blood analysis is within normal parameters. Full blood count shows mild anemia. There is no leukocytosis. Clotting times are normal. There is no thrombocytopenia. The patient is referred to the hospital for urgent CT scan. Collections of subdural blood can be identified in various regions, predominantly occipital. The patient is admitted to the ICU.
|
 Ophthalmological emergencies
Ophthalmological emergencies